The Omicron wave of COVID-19 has caused record case numbers and a related surge in hospitalizations across Tennessee. This brief demonstrates how current high numbers of COVID-19 hospitalizations affect access to hospitals for every Tennessean, not just those in need of specialized care for COVID-19.
It remains true that the unvaccinated and immunocompromised individuals face higher risks of severe outcomes despite evidence that the omicron variant produces less severe disease in most people. This fact, coupled with the sheer number of cases flooding the state, means that Tennessee hospitals, again, are facing significant strain to care for all patients, not just those suffering from COVID-19.
In practical terms, fewer available staffed hospital beds means all patients who need care, like those who have been injured in a car accident or experienced a heart attack, may face delays or the inability to access a preferred hospital. So far, no comprehensive data have been available to suggest how timely access to care for all Tennesseans has been affected by surges in hospitalizations for COVID-19.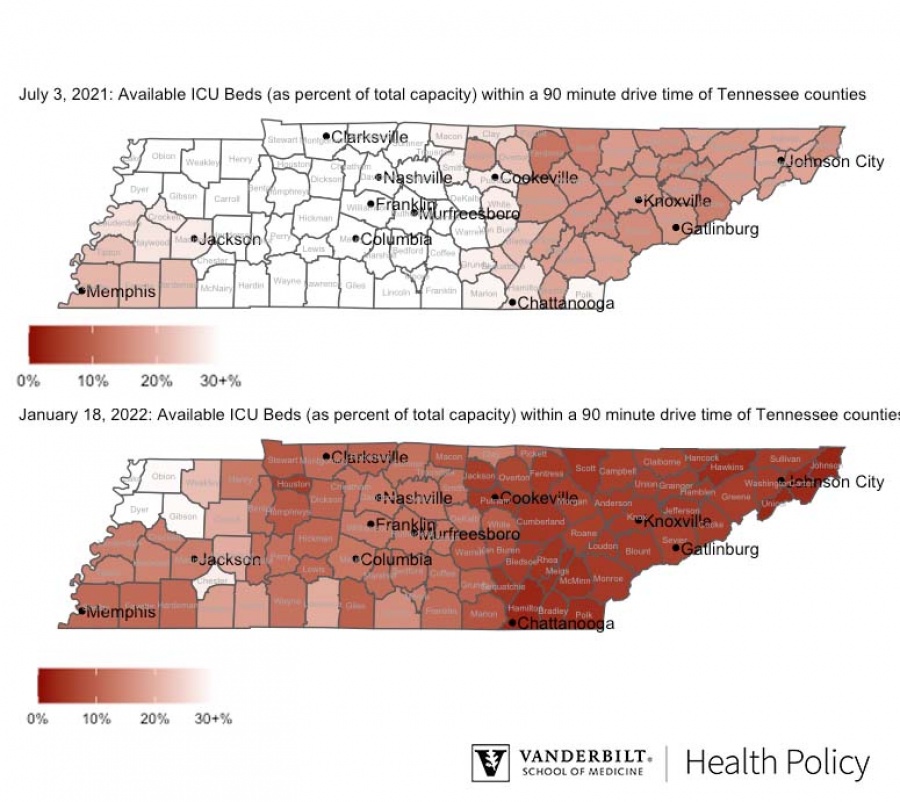
Figure 1 illustrates the current capacity crunch, specifically, the percentage of available ICU beds within a 90-minute drive time of the most populated area of each county within the state. Because 100% ICU bed availability is not realistic, we benchmark current drive times against those in early July 2021, just prior to the delta variant surge and when COVID-19 hospitalizations reached their lowest point since the early days of the pandemic.
The situation today stands in stark comparison to early summer 2021. In only one area of the state (Northwest Tennessee, along the Missouri-Arkansas border) is ICU capacity at a similar level — though we caution this result is averaged across hospitals (including out-of-state hospitals near borders with neighboring states) within a 90 minute driving radius of an area, and this average may not represent availability at individual facilities. In almost every county of Tennessee, substantially fewer critical care beds are currently available to Tennesseans within a 90-minute drive.
An alternative way to present the same data is by asking a simple question: “How much longer would a Tennessean have to drive right now, in January 2022, to reach a hospital with a staffed ICU bed than they would have driven in early July 2021?”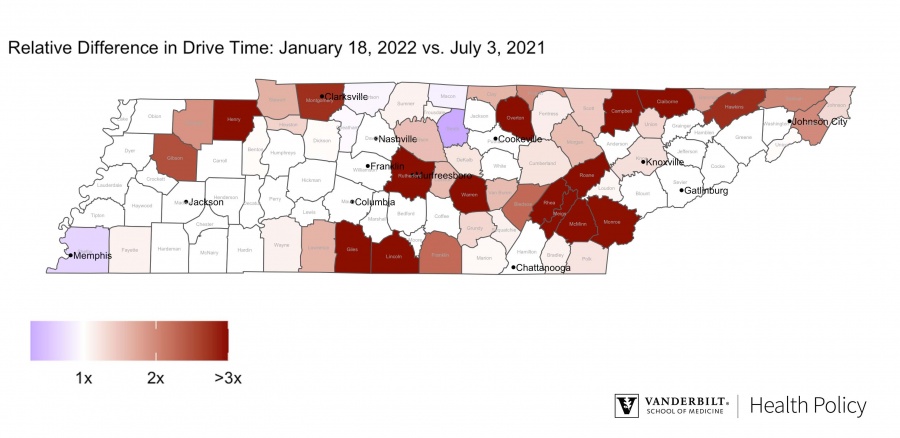
Figure 2 shows estimates for each county of the state. In this figure, we see that in certain areas of the state, drive times are 3 times longer or more now than they were in Summer 2021.
While the current hospitalization outlook is poor, continued vigilance — vaccination, masking, testing, and distancing when appropriate — can support the capacity of the Tennessee health care system to provide timely and quality care to all patients during this surge, both those hospitalized for COVID-19 and all others in need of hospital care.