(The following was originally published by the VUMC Communications Office.)
Medicare Part D enrollees may pay more out of pocket for high-priced specialty generic drugs than their brand-name counterparts, according to new research by health policy experts at Vanderbilt University Medical Center and the University of North Carolina at Chapel Hill.
Researchers examined differences in brand-name and generic or biosimilar drug prices, formulary coverage and expected out-of-pocket spending across all of the Medicare Part D plans available in the United States in the first quarter of 2018.
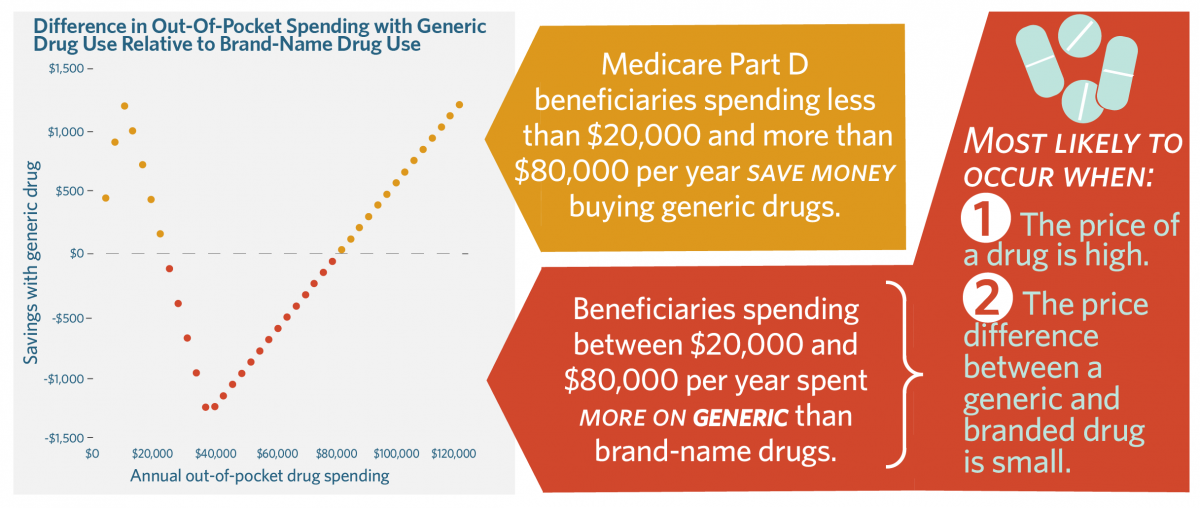
The study, published in the July issue of Health Affairs, found that current Medicare Part D beneficiaries can have higher out-of-pocket spending for generics than their branded counterparts if they use expensive specialty drugs and if the price differences between brands and generics are not large. This can be common for individuals prescribed specialty drugs typically used to treat rare or complex conditions such as cancer, rheumatoid arthritis or multiple sclerosis.
“Ironically, even if we assume that generic drugs have lower list prices than brands, for Medicare beneficiaries with $20,000 to $80,000 in annual drug spending, using only brand-name drugs could actually save them money,” said Stacie Dusetzina, PhD, associate professor of Health Policy and Ingram Associate Professor of Cancer Research at VUMC, the study’s lead author.
READ THE HEALTH AFFAIRS STUDY HERE: https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05476
“This is happening because branded drug manufacturers now pay a discount in the donut hole, which gets counted as out-of-pocket spending,” she said. “This helps patients reach catastrophic coverage faster, where they pay 5% of the drug’s price instead of 25%. Generic drug makers do not pay these same discounts, so patients have to spend more of their own money to make it to the catastrophic phase of the benefit.”
In 2019, this means people using brand-name drugs who reach the donut hole, or coverage gap, have to spend $982 to get to the catastrophic coverage phase. People using generic drugs have to spend $3,730 to reach that point. The study also notes policy changes set to take effect in 2020 will only make the situation worse by increasing patient out-of-pocket spending requirements for the catastrophic phase coverage from $5,100 to $6,350.
In response, the administration of President Donald Trump and the Medicare Payment Advisory Commission (MedPAC) have included recommendations to exclude the manufacturer discount from out-of-pocket spending calculations.
“While this would level the playing field between generic drugs and brands, it would do so by making brand-name drugs more expensive instead of making generic drugs less expensive,” said Dusetzina. “Congressional committees have signaled interest in addressing this and other issues in Medicare Part D, including placing a cap on out-of-pocket spending.
“The Part D benefit needs a redesign so that it works for people needing expensive drugs. I hope Congress will take this opportunity to make changes to Part D, including making sure that generic drug users aren’t overpaying for these drugs.”
In addition to Dusetzina, study authors are Shelly Jazowski, a doctoral student in the Department of Health Policy and Management at the University of North Carolina at Chapel Hill (UNC-Chapel Hill) and predoctoral fellow in the Department of Population Health Sciences at Duke University; Ashley Cole, a fellow at the Cecil G. Sheps Center for Health Services Research at UNC-Chapel Hill; and Joel Nguyen, a doctoral student in the UNC Eshelman School of Pharmacy at UNC-Chapel Hill.