Modernizing health records by making them electronic has gained momentum as technology evolves and policies push health care toward digital solutions. But the same trend has not been evident for physicians who remain in private practice, new research finds.
The research led by Jordan Everson, PhD, assistant professor in the Department of Health Policy at Vanderbilt University Medical Center (VUMC), finds striking differences in use of electronic health records (EHRs) among more than 291,000 physicians included in the study.
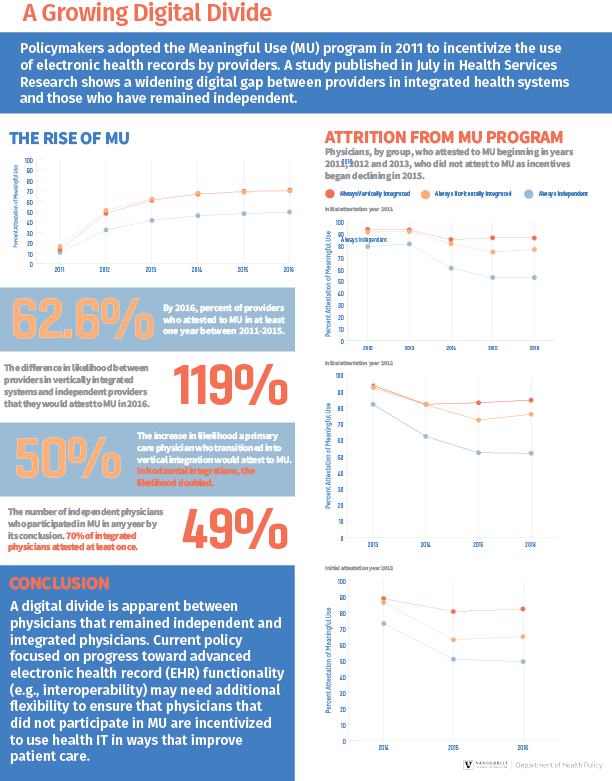
Forty-nine percent of physicians who had remained independent since 2011 and were surveyed in the study attested to Meaningful Use of EHRs, such as electronic prescribing of medications and online patient portals -- at least once. In contrast, 70% of doctors in both group practices and working for hospitals during the study's timeline attested to meaningful use.
Meaningful Use of EHRs was first defined in 2009 by the America Reinvestment & Recovery Act, and financial incentives were offered to physicians and health systems that serve Medicare and Medicaid patients. The program was voluntary, and after 2015 the Centers for Medicare and Medicaid Services (CMS) began reducing payments to providers if there was no expansion in adoption of EHR Meaningful Use practices.
Everson said this can be interpreted in several ways. One is independent doctors have more authority over the technology they use and could simply choose not to continue in the program as opposed to doctors in integrated systems where management could require participation.
"Another way to interpret this is that the cost-benefit equation was worse for independent physicians," Everson said. "In other words, the financial incentives in later years were not enough to overcome the cost of keeping up with Meaningful Use in addition to the time burden of using EHRs. Financial costs are likely particularly high for independent physicians who can't spread the cost across a large organization."
About half of independent physicians who participated in the EHR incentive program in the first years -- 2011 through 2013 -- left the program by 2015. In the same time frame, less than 20% of physicians who worked for hospitals left the program.
The study highlights other possible factors in this trend, such as an aging independent physician population that is retiring in greater numbers.
And while doctors have been moving into larger, integrated health practices for decades as the U.S. health system has grown more complex, that option might not be available for physicians that haven't kept up with new technologies. The study showed that independent physicians who participated in Meaningful Use on their own were more likely to later join integrated systems than physicians who did not participate.
"That may mean that physicians who are not technologically savvy do not have the option to join a bigger system to get help with new technologies," Everson said.
Everson's research, conducted with Melinda Buntin, PhD, Mike Curb Chair of Health Policy at Vanderbilt, and Michael Richards, MD, PhD, an associate professor at Baylor, is the most recent in a number of studies that have illustrated challenges faced by independent practices in adopting new and costly technology, or what many clinicians describe as physician burnout with electronic records.
Read the study, published in Health Services Research by clicking here.