A new study published in the medical journal BMJ finds that oncologists who received payments from the pharmaceutical industry were more likely to give patients prescriptions for cancer drugs that are less effective or more expensive.
Authored by Aaron Mitchell, an oncologist and researcher at Memorial Sloan Kettering Cancer Center and Stacie Dusetzina, Ingram professor of Cancer Research and Health Policy at Vanderbilt University Medical Center, the study examined four low-value cancer treatments using a database of payments from drug manufacturers to oncologists. These payments most commonly come in the form of free meals, speaking or consulting fees.
The pharmaceutical industry gives physicians over $2 billion in non-research related payments annually, researchers said. Many previous studies have demonstrated that these payments influence physicians.
“We know from previous research that industry payments can sway doctors between equivalent treatment options, but this study is the first to show these payments can lead to cancer treatments that are not recommended, or even potentially harmful to some patients,” Mitchell said.
The treatments included in the study were:
- denosumab for castration-sensitive prostate cancer;
- granulocyte colony stimulating factors (GCSF) for patients at low risk for neutropenic fever;
- nab-paclitaxel for cancers with no evidence of superiority over paclitaxel, or;
- a branded drug in settings where a generic or biosimilar version was available.
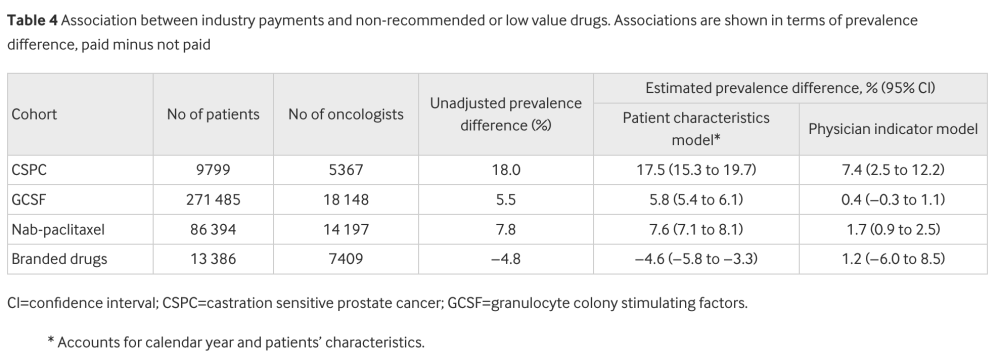
For three of the four cancer treatments, the proportion of patients who received the unhelpful or more expensive drug was higher among oncologists who received payments from drug makers in unadjusted analyses, researchers noted.
When adjusted for physician characteristics, two treatments – non-recommended denosumab for prostate cancer, and Abraxane, a more expensive brand-name drug known generically as paclitaxel – were prescribed significantly higher. The other two treatments were not significantly different after adjustment.
In adjusted analyses, industry payments were associated with a 7%% increase in the prescription of denosumab and a 2% increase in the prescription of nab-paclitaxel.
Dusetzina said the findings raise quality-of-care concerns regarding financial relationships between drug makers and physicians.
“Industry payments to physicians clearly influence physician prescribing – and not necessarily for the better. We may need to consider limits on the types and frequency of physician-industry financial interactions as it isn’t clear that these interactions are beneficial for patients. ”
The research was funded by grants from the National Cancer Institute, National Institute of Health Care Management, and Memorial Sloan Kettering Cancer Center.