Type 1 diabetes mellitus (DM) patients manifest an increased incidence of heart failure (HF) after incident myocardial infarction (MI). Unfortunately, a "therapeutic deficit" exists in the treatment and prevention of post-MI HF in the setting of type 1 DM. This is due in large part to the fact that management approaches to cardiovascular disease reduction have been extrapolated in large part from experience in type 2 DM, despite the longer duration of disease in type 1 DM than in type 2 DM and important differences in the underlying pathophysiology. To that end, we have previously shown that after MI, type 1 DM is associated with accentuated myocardial oxidative stress (OS) and concomitant worsening of residual left ventricular (LV) function. However, the molecular mechanisms by which type 1 DM-enhanced OS adversely affects HF after MI remain poorly understood.
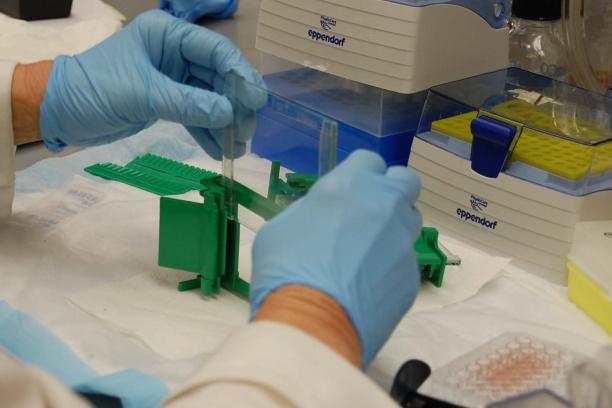
To address this issue, research activities in our laboratory are directed towards improving our understanding of OS-mediated mechanisms of myocardial injury and degeneration after MI in the type 1 diabetic heart and to use this knowledge to develop novel anti-oxidative therapies for the prophylaxis of post-MI HF potentiated by type 1 DM. Studies performed in our laboratory utilize the streptozotocin (STZ)-diabetic rat in a well-established rat model of HF due to MI by coronary artery ligation as well as human specimens from type 1 diabetic patients with a history of MI. The injection of STZ in rats leads to the development of hyperglycemia, excessive urination, and loss of weight, all of which mimics human type 1 diabetes. A broad multidisciplinary approach encompassing diverse techniques (integrative, physiology, protein chemistry, biochemistry, immunohistochemistry, proteomics, imaging mass spectrometry, pathology, and histology) allows for integration of proteomic and biochemical information at the molecular level with physiological information at the whole animal level.
This molecular physiologic strategy is currently being used to identify OS induced-post-translational modifications (OSi-PTMs) of cardiac proteins in failing rat and human diabetic post-MI hearts that are known to confer loss of function and result in reduction in the healthy myocardial protein pool, thereby negatively impacting myocyte survival and function. This multidisciplinary approach is also being used to characterize the significance of lipid peroxidation-derived reactive electrophiles and lipid electrophile protein adducts as downstream mediators and determinants of oxidant injury in the type 1 diabetic heart following MI and during subsequent HF. Evaluation of therapies preventing interactions of secondary products of OS with target proteins may help inform the clinical care of type 1 diabetics who have suffered a myocardial infarction.