Welcome to the Adult Cleft and Craniofacial Program at Vanderbilt University Medical Center. Whether you have graduated from a pediatric cleft and craniofacial program, are recovering from a traumatic injury or illness, or are unhappy with the appearance of your head or face for any reason, we are here to help.
As one of the first in the nation, the Adult Craniomaxillofacial Surgery Program consists of a group of experts highly skilled in cosmetic and reconstructive surgery of the scalp, face, teeth and everything in-between.
Please feel free to e-mail us at craniofacial@vumc.org with any questions you may have. We look forward to meeting you and helping you become the best version of yourself.

Matthew Pontell, MD
Assistant Professor of Plastic Surgery
Department of Plastic Surgery
Academic Pursuit of Excellence in Craniomaxillofacial Surgery
At the Adult Craniomaxillofacial Surgery Program, we pride ourselves in practicing evidence-based medicine and surgery. Our team members are highly active in national and international societies, and frequently publish in high-impact, well-respected, peer-reviewed journals. See Dr. Pontell's publications on PubMed
Societies We Are Members Of:
- AO Craniomaxillofacial - https://www.aofoundation.org/cmf
- American Society of Craniofacial Surgeons - https://ascfs.org
- International Society of Craniofacial Surgery - https://iscfs.org/
- American Cleft Palate Craniofacial Association - https://acpacares.org/
- The American Society of Maxillofacial Surgeons - https://maxface.org/
Journals We Publish In:
- Plastic & Reconstructive Surgery - https://journals.lww.com/plasreconsurg/pages/default.aspx
- Journal of Craniofacial Surgery - https://journals.lww.com/jcraniofacialsurgery/pages/default.aspx
- FACE - https://journals.sagepub.com/home/FAC
- Journal of Oral & Maxillofacial Surgery - https://www.joms.org/
- Annals of Plastic Surgery - https://journals.lww.com/annalsplasticsurgery/pages/default.aspx
Nashville Predators On-Site Surgeons
As members of the Nashville community, we share our city’s pride for our sports teams. Our team provides Adult Craniomaxillofacial Surgery Services to the Nashville Predators during games, and we are available for the treatment of any problems that may arise afterwards.
Let’s Go Preds! |
 |
 |
 |
 |
| Stephane Braun, MD Associate Professor of Clinical Plastic Surgery Department of Plastic Surgery |
Michael Golinko MD, FACS, FAAP Associate Professor of Plastic Surgery, Neuroglogical Surgery, and Otlaryngology Chief of Pediatric Surgery Director of the Pediatric Cleft & Craniofacial Program, Department of Plastic Surgery Assistant Professor, Neurological Surgery |
Meagan Vucovich, MD Assistant Professor of Plastic Surgery Department of Plastic Surgery |
Academic studies and treatment solutions
Facial Trauma
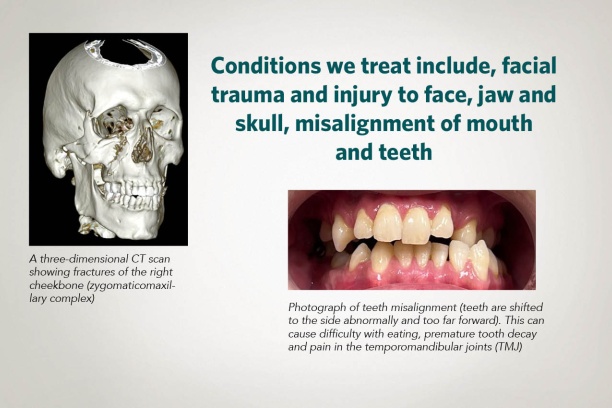
Craniomaxillofacial trauma is extremely common with over 25% of nationally reported injuries involving the face1. A 2020 publication reported over 7.5 million facial fractures in one year alone2. Injuries range from simple skin cuts to complex skeletal fractures involving the nerves, teeth, eyes or even the brain.
Issues arising from these injuries can require treatment right away, or even years later. Almost every procedure we offer has implications in the management of craniomaxillofacial trauma.
|
Image 1: 3D CT scan showing right cheekbone fractures (zygomaticomaxillary complex). Correction often requires cheekbone reconstruction. |
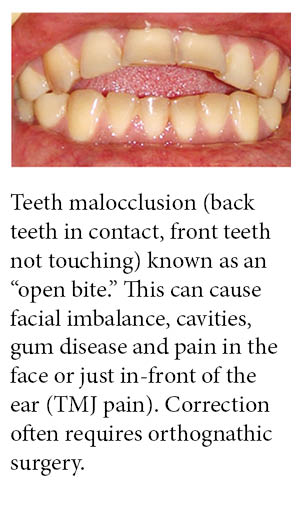
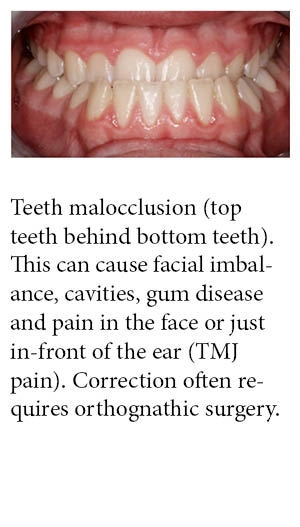
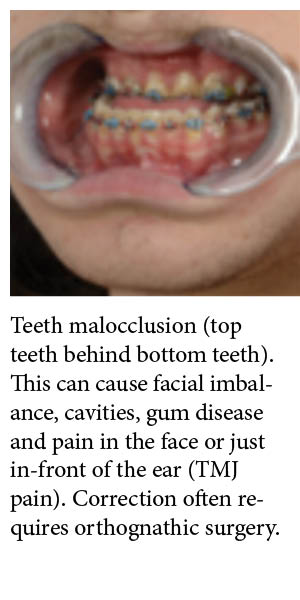
Image 2: Teeth malocclusion (top teeth behind bottom teeth). This can cause facial imbalance, cavities, gum disease and pain in the face or just in-front of the ear (TMJ pain). Correction often requires orthognathic surgery. |
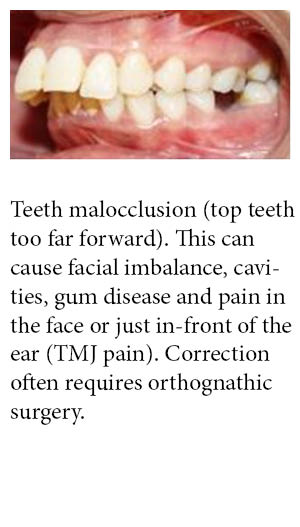
Image 3: Teeth malocclusion (teeth are shifted to the side and too far forward). This can cause facial imbalance, cavities, gum disease and pain in the face or just in-front of the ear (TMJ pain). Correction often requires orthognathic surgery. |
- References:
- Choi J, Lorenz HP, Spain DA. Review of facial trauma management. J Trauma Acute Care Surg. 2020 Apr;88(4):e124-e130. doi: 10.1097/TA.0000000000002589. PMID: 31972757. https://pubmed.ncbi.nlm.nih.gov/31972757/2.
- Lalloo R, Lucchesi LR, Bisignano C, et al. Epidemiology of facial fractures: incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj Prev. 2020;26(Supp 1):i27-i35. https://pubmed.ncbi.nlm.nih.gov/31915268/
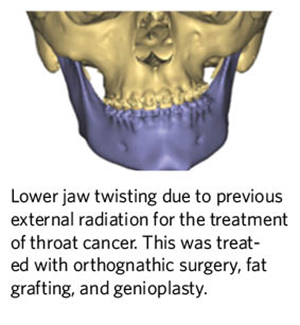
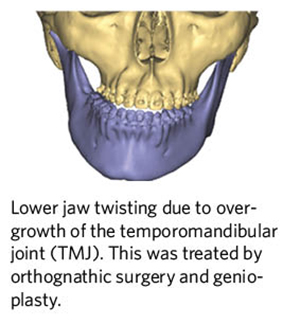
Jaw Dysfunction
Dysfunction of the upper and/or lower jaws has a variety of causes including temporomandibular joint (TMJ) dysfunction, congenital dento-facial abnormalities and issues that arise after treatment of trauma, cancer or other pathologies.
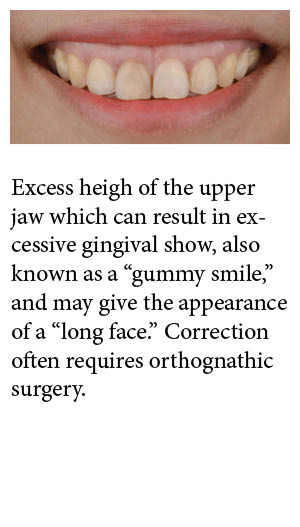
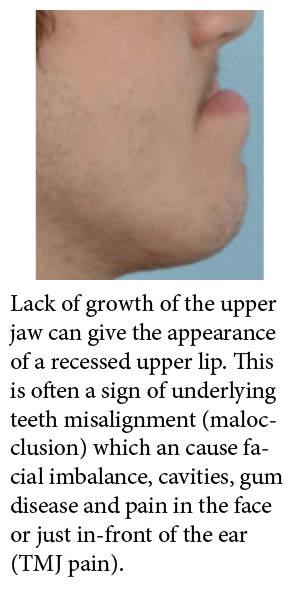
Jaw dysfunction can be accompanied by abnormal alignment of the teeth, or malocclusion, which can result in facial imbalance, cavities, gum disease and pain in the face or just in-front of the ear (TMJ pain). Jaw dysfunction can also result in poor self-esteem and anxiety around the overall appearance of the face jaw dysfunction can often be treated with orthognathic surgery.
|
|
|
|
|
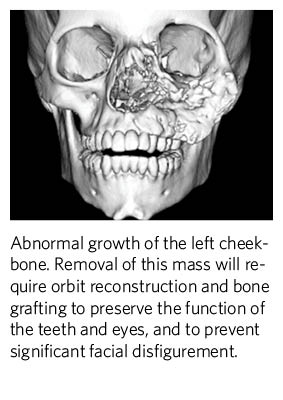
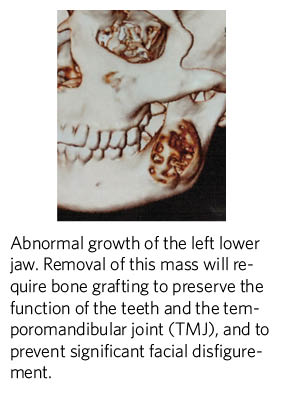
Jaw Tumors
- Many different types of growths, benign and malignant can be found in the upper or lower jaw.
- Initial treatment may involve removal of the tissue, which can leave a patient with profound functional and aesthetic issues if not reconstructed appropriately.
- Many treatment options are available at the time of mass removal such as bone grafting.
- Issues arising years after the initial reconstruction can often be corrected by bone grafting, fat grafting, or orthognathic surgery.
|
|
|
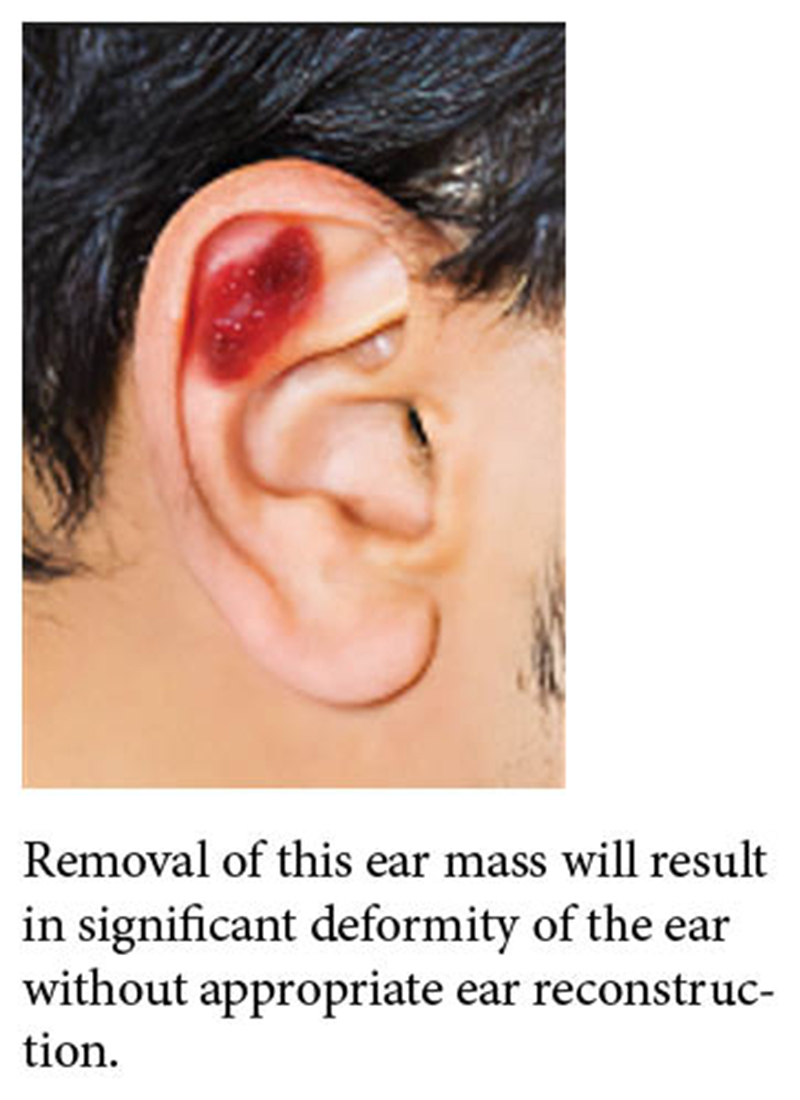
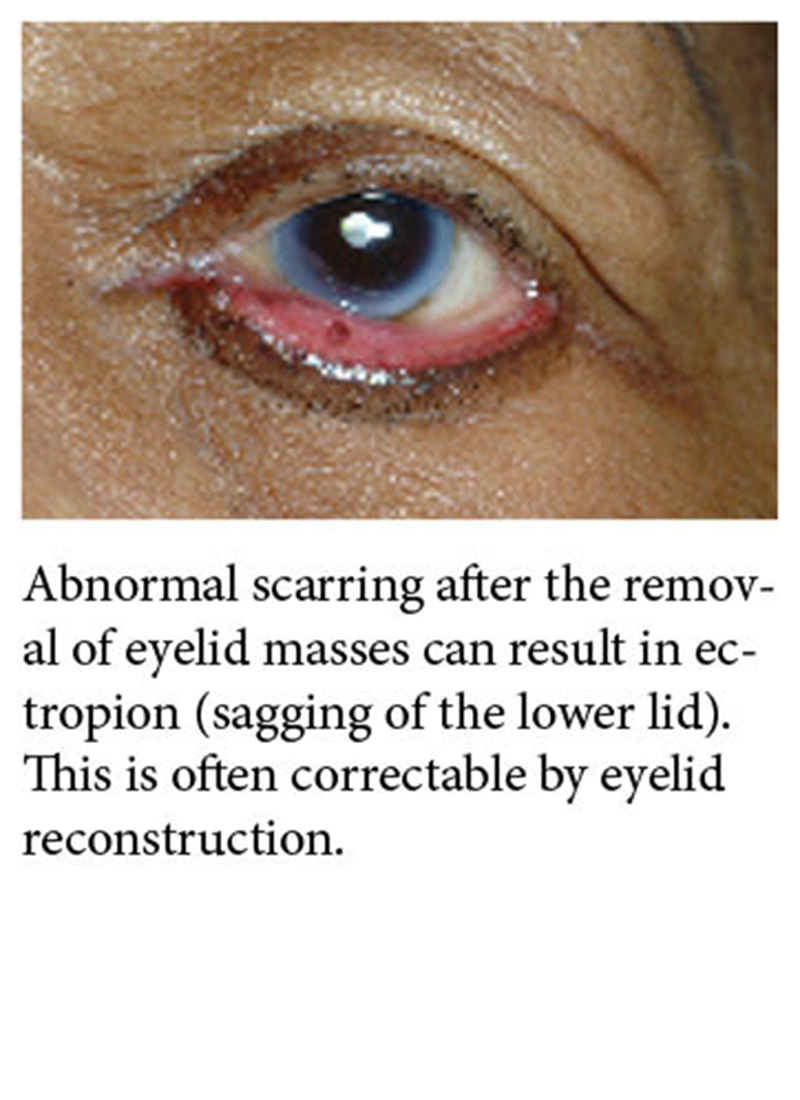
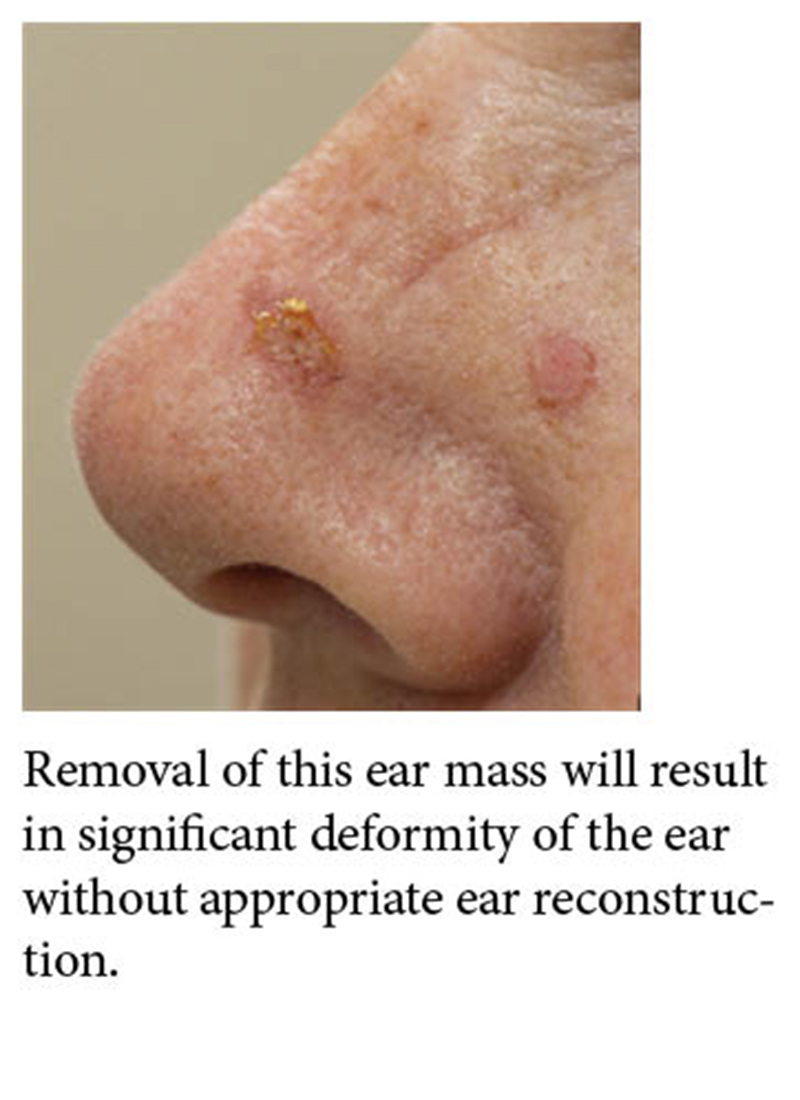
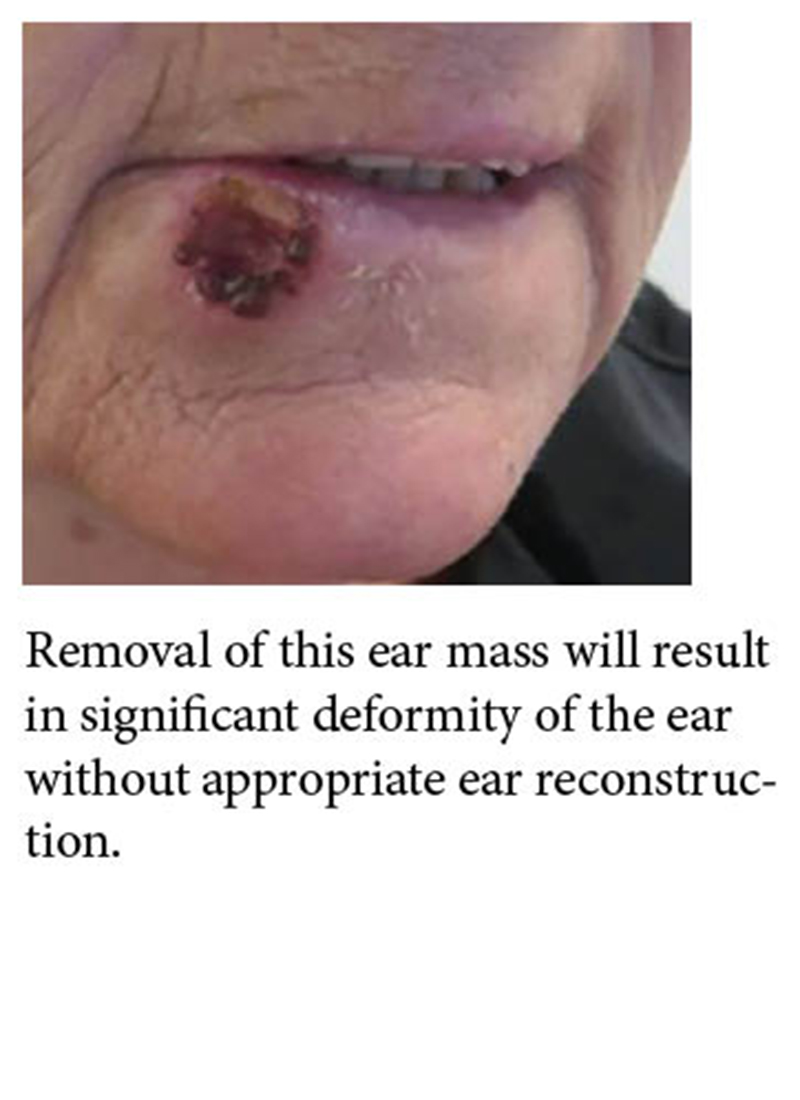
Facial Masses and Scarring
Benign and malignant tumors can arise anywhere on the face or ears.
Mass removal can result in significant facial disfigurement if not reconstructed appropriately immediately after removal.
Issues can arise years later from unexpected consequences of the initial reconstructions.
Unsightly scars can be revised at any time by facial reconstruction.
 |
 |
 |
 |
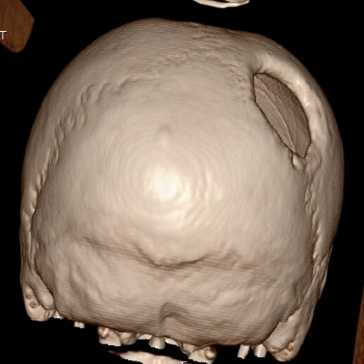
Scalp Masses and Scarring
- Benign and malignant tumors can arise anywhere on the scalp.
- Mass removal can result in significant hair loss (alopecia) or unsightly scars.
- Masses that involve the bone may also require cranium (skull) reconstruction.
|
Patches of hair loss (alopecia) can result from trauma, prior surgical procedures or other pathologies. Often times they can be treated with scalp reconstruction. |
Defects in the skull can result from trauma or surgery, placing the underlying brain at risk. These defects are often treatable by cranium (skull) reconstruction. |
Facial Pain
- Pain in the head and face is common and can arise from any number of issues such as unrecognized growths, trapped nerves, abnormal scars, an abnormal bite (malocclusion) and temporomandibular joint (TMJ) dysfunction.
|
Teeth are shifted to one side causing an abnormal bite (malocclusion) that is causing this patient temporomandibular (TMJ) pain, which is often present just in-front of the ear. This is often correctable with orthognathic surgery. |
Absent Eye
- Patients who have had their eyeball removed (enucleated) for trauma or another illness can often develop difficult wounds in the eye socket.
- These wounds can result in the inability to receive a prosthetic eye.
- After orbit reconstruction, patients are often able to go on to receive a prosthetic eye.
|
A patient who suffered the traumatic loss of the right eye with exposed reconstructive hardware. This wound is not suitable for a prosthetic eye and requires further orbit reconstruction. |
Cleft Lip and Palate
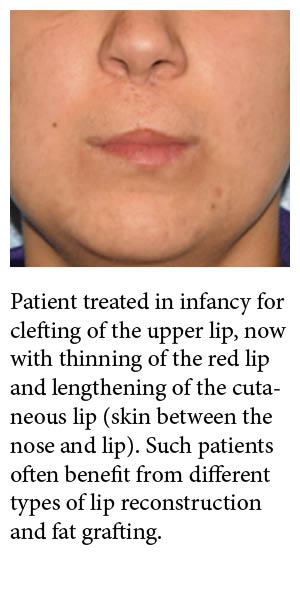
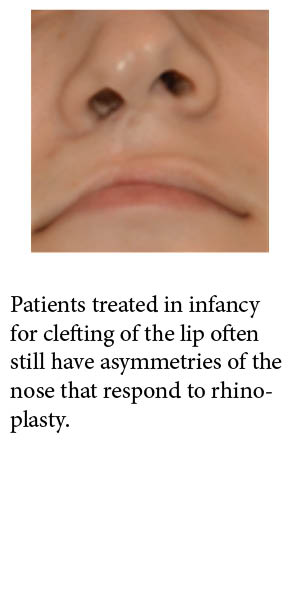
- Patients with cleft lip and palate undergo several surgeries throughout life
- Many patients may still be unhappy with the appearance of their upper lip and may benefit from lip reconstruction or fat grafting.
- Patients may also have persistent nasal disfigurement and nasal airway obstruction that is often responsive to rhinoplasty.
- Patients also may develop teeth misalignment (malocclusion) which can cause facial imbalance, cavities, gum disease and pain in the face or just in-front of the ear (TMJ pain). Facial imbalance can result in poor self-esteem and anxiety around the overall appearance of the face.
 |
 |
 |
 |
Facial Asymmetry (Hemifacial Microsomia/Parry Romberg Syndrome)
- Facial asymmetry can result from conditions such as hemifacial microsomia or Parry Romberg syndrome, or from prior trauma or illness.
- Irrespective of the cause, many treatment options exist to improve symmetry.
- Bony deficiencies can be treated by bone grafting, and soft tissue deficiencies can be treated by fat grafting.
- Additional procedures used to achieve symmetry include rhinoplasty, orthognathic surgery, and genioplasty.
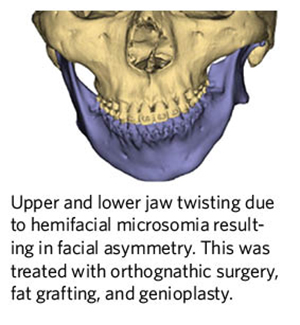 |
 |
 |
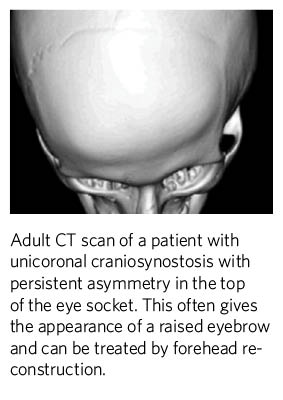
Craniosynostosis
- Patients born with craniosynostosis often undergo surgery on the skull during infancy and throughout adolescence.
- Patients go on to develop asymmetry of the eyes that is often treatable by forehead reconstruction.
- Characteristic deformities of the sides of the forehead are also treatable by cranioplasty, fat grafting and forehead reconstruction.
- Defects of the skull can be treated by cranioplasty and poor scarring can be treated by scalp reconstruction.
- Patients with complex forms of craniosynostosis, such as Crouzon, Pfeiffer or Apert syndrome, often benefit from the above procedures which can also correct prominent eyes (exorbitism).
 |
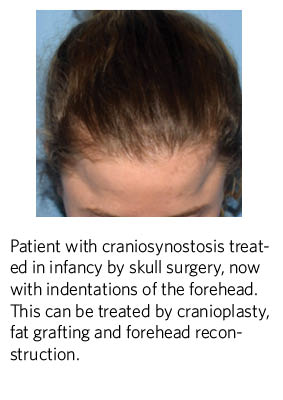 |
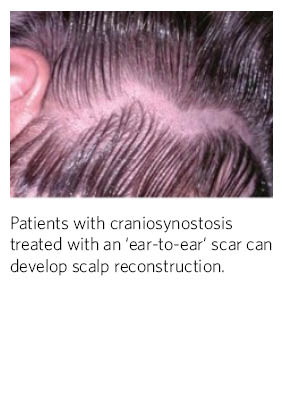 |
Fibrous Dysplasia
- Fibrous dysplasia results in abnormal bone formation.
- Bone growth can cause facial disfigurement and malposition of the eyes affecting vision.
- The deformities caused by fibrous dysplasia can be treated by various techniques to improve facial symmetry and alignment of the eyes.
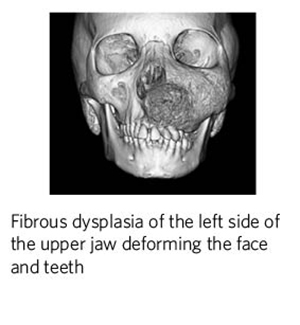 |
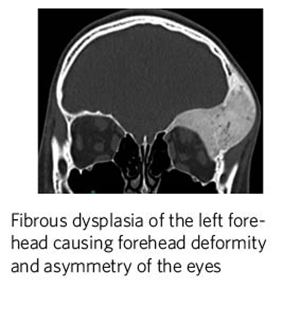 |
Treacher Collins Syndrome
- Patients with Treacher Collins syndrome often have a distinct position of the eyelids that can be adjusted by orbital reconstruction.
- The cheek region can be augmented by cheek reconstruction or fat grafting.
- The upper and lower jaws can be positioned in a way that makes it hard to breathe, causing obstructive sleep apnea. This can often be improved by orthognathic surgery and genioplasty.
 |
 |
Obstructive Sleep Apnea
- Patients with obstructive sleep apnea (OSA) who have not responded to other surgical and non-surgical treatments, may benefit from orthognathic surgery
- Moving the jaws (orthognathic surgery) can help open the airway for some patients, alleviating the symptoms of obstructive sleep apnea (OSA).
- In certain patients, moving the chin bone (genioplasty) can also have beneficial effects on airway function.
- Orthognathic surgery and genioplasty surgery have helped some patients discontinue the use of positive pressure ventilation (i.e. CPAP).