Click on one of the topics below or proceed to forms.
Conduct periodic control checks to monitor the prompted voiding program and ensure quality of care. Share results with nurse aides to elicit their help with improvement efforts and strengthen their commitment to the program.
-
Having accomplished Step 1, Step 2 and Step 3, your facility now has a significant investment in improving the quality of incontinence care for residents. All that time and effort may go to waste, however, unless supervisors conduct regular “wet” checks to make sure nurse aides continue to provide toileting assistance. Most nursing homes forego this step only to pay a price for their negligence: studies show that in the absence of quality control assessment, nurse aides backslide (or new staff are not trained in prompted voiding) and fail to consistently implement prompted voiding with incontinent residents (1).
-
Quality monitoring starts with conducting quality control checks—also called wet checks. This is a four-step task that takes about 15-20 minutes per week:
Weekly Wet Check Procedure- Once a week, a supervisory nurse should check a random sample of at least 10 prompted voiding residents for wetness. How do you identify a random sample? Write the names of each prompted voiding resident on a slip of paper, put all the slips in a hat, and pull 10. Make sure the wet checks are unpredictable. Don’t, for example, always conduct them on the same day at the same time.
- Record wet check results on our Wet Check Record. Use the results to calculate a weekly wetness rate. For example, if two of the 10 residents are found wet, then the wetness rate for that week is 20%.
- Report the results to CNAs. A 5-minute stand-up meeting will do. As a general rule, if the wetness rates exceeds 30% (that is, if 4 or more of the 10 residents are wet or soiled), then the prompted voiding program is not working as expected. Ask CNAs for improvement recommendations. If the wetness rate is 30% or lower, congratulate them on a job well done.
-
You can fine tune wet checks by calculating a Wet Check Warning Limit that takes into account the toileting rates of the residents in your facility. In the above, general procedure, we used a 30% wetness rate at the default Wet Check Warning Limit. In fact, however, depending on your residents, a higher or lower warning limit may be more appropriate. We won’t go into the statistical rules used to calculate a customized Wet Check Warning Limit. There’s no need, for we created an Excel program that will do those calculations for you.
-
For best results, keep track of the wet check results over time. A visual chart of results will help you spot patterns easily.
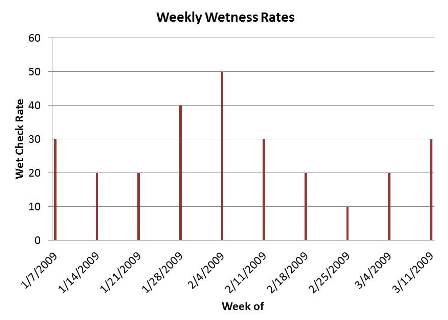
Is performance improving? Staying the same? Declining? In the example above, the wet-check pattern suggests the prompted voiding program is working as expected, with the exception of a two-week period starting the week of 1/28/18. If high wetness rates become a frequent or consistent problem, further analysis is need. Consider, for example, whether out-of-control results indicate a change in a resident’s status, a breakdown in care during shift changes, or a staffing problem (e.g., turnover, new hires, agency workers) on a particular hallway. All these are common occurrences that can skew program results.
Over the course of several weeks, as prompted voiding becomes routine for the staff and residents, you should see consistent wet check results. After several months of consistent results, you can consider conducting random wet checks bi-weekly. But don’t stop them! In addition to the performance feedback they provide, the wet checks send a message to CNAs that the facility values high-quality incontinence care. This helps keep motivation levels high and sets expectations for new staff.
-
This step bears repeating, for continuous quality improvement to work, you must share wet check results with the CNAs or other staff responsible for the daily delivery of the prompted voiding program. As we noted at the start of this step, staff members need feedback—both good and bad—to help them establish new work routines. Simply posting an updated control chart each week, for example, will enable nurse aides to make connections between their work and the impact it has on their residents. If CNAs can see tangible evidence of the prompted voiding program’s benefits, then they are less likely to view the intervention as an additional burden and more likely to work to sustain its positive effects.
Sharing performance results also gives nurse aides the opportunity to help supervisors correct any problems that arise. Often the aides are the first to know if a resident’s status has changed or if there’s been a break-down in the work process. Involving these staff members in improvement efforts will also help strengthen their commitment to the program.
In addition to posting control charts, you can present wet check results at in-service trainings and regular staff meetings. A 5-minute stand-up meeting once a week focused specifically on incontinence care is effective for training and management purposes.
Consider rewarding the staff for consistently good results. The most powerful motivators are job advancements and salary increases. If these are beyond your budget, a staff pizza party every quarter for outstanding performance can’t hurt.