-
Tennessee Poison Center has partnered with the Tennessee Pharmacists Association (TPA) to promote the use of a Universal Medication List. The goal of the project is to improve medication safety in Tennessee by providing a universally consistent process for communicating vital patient information regarding medications and allergies across the continuum of care.
This form will enable patients to carry an up-to-date medication and allergy list with them at all times. It will ensure availability at entry and exit from all healthcare encounters.
To download a copy of this form, please visit the TPA website: www.tnpharm.org
-
Internet Pharmacies - Buyers Beware
Using the internet is a convenient way to purchase products. Buying prescription medications is no exception; however, not all website “pharmacies” are licensed, and some are not pharmacies at all.
They are websites designed to gather personal information about you and obtain credit card information. Even if the website sends you a product, the medication may be fake or expired.
The Food and Drug Administration (FDA) provides information about using online pharmacy services wisely, including guidelines and tips on using online resources to purchase your prescriptions.
The National Association of Boards of Pharmacy is a national organization of the individual State Boards of Pharmacy. This has a program to help you learn if a pharmacy website is meeting the required regulations. To verify if a pharmacy website has met the state and federal regulations to sell medicine online, go to Verified Internet Pharmacy Practice.
These issues are not limited to prescriptions for human medications. There is a recent newsletter from the FDA regarding fraudulent websites that claim to sell drugs for pets. Unfortunately, some of these sites are selling counterfeit products or expired medications which could be dangerous to your pet. More information about this including tips for ordering your pet’s medications online can be found on the FDA website here.
FDA 101: Health Fraud Awareness
The FDA has produced an information resource on health fraud called FDA 101: Health Fraud Awareness. For more information, click here to visit the website.
-
What Can I do With Old and Unused Medicine?
Flushing medicine down the sink or toilet may be bad for the environment. Throwing it away with the trash may cause less pollution, but there is a risk that other people or animals may find it. Privacy may also be a concern if containers have labels with names and other personal information.
The following steps can be taken to more safely dispose of unused and expired medication:
- Keep medications in the containers they came in with child-resistant lids firmly in place.
- Remove labels before discarding the medication or use a permanent marker to cover any personal information on labels.
- If throwing away liquids, place the liquids in a plastic bag that can be sealed in case of leaks. Wrap glass bottles to prevent breakage.
- Mix medication with things like coffee grounds so people will be less likely to take them.
- Add a small amount of water to pills or capsules to at least partly dissolve them.
- Put the medication inside a package such as a box that doesn’t show what’s inside.
- Put the medication in the trash as close to pick up time as possible – do not put in recycling bins.
The Tennessee Department of Environment and Conservation Office of Sustainable Practices has a program providing guidance and assistance related to the proper management of unwanted household waste. Click here for details.
-
Could you accidentally poison yourself by taking over-the-counter (OTC) products?
Hundreds of senior citizens in Tennessee call Tennessee Poison Center after taking herbal medications, dietary supplements, vitamins, pain relievers, antihistamines, cough/cold therapies or gastrointestinal remedies. Why did those people call? Reasons included:
- Feeling ill after taking OTC products with prescription medicine
- Taking an extra dose
- Taking someone else’s medicine
- Discontinuing prescription medicine and substituting OTC medicine
- Taking higher-than-recommended doses of OTC medicine
Information about Interactions
An interaction refers to a problem that occurs when a medication is combined with another medication, food or alcohol. That doesn’t just refer to combinations taken at the exact same time. Some interactions can occur even if the two items are spaced many hours apart.
Grapefruit and medication interactions
Avoid grapefruit or grapefruit juice unless approved by your pharmacist. Grapefruit juice interferes with enzymes that break down certain drugs in your digestive system. If components of your medicines build up, you may have abnormally high blood levels of these drugs and an increased risk of serious side effects. The exact chemical or chemicals in grapefruit juice that cause this interaction can be in the pulp, peel and juice of grapefruit as well as in dietary supplements that contain grapefruit bioflavonoids. Until proven safe, do not take grapefruit if you are on the following medications:
- Carbamazepine (Carbatrol, Tegretol)
- Buspirone (BuSpar) clomipramine (Anafranil) and sertraline (Zoloft)
- Diazepam (Valium), triazolam (Halcion)
- Felodipine (Plendil), nifedipine (Adalat, Procardia), nimodipine (Nimotop), nisoldipine (Sular) and possibly verapamil (Isoptin, Verelan)
- Saquinavir (Fortovase, Invirase) and indinavir (Crixivan)
- Simvastatin (Zocor), lovastatin (Mevacor) and atorvastatin (Lipitor), simvastatin-ezetimibe (Vytorin)
- Cyclosporine (Neoral, Sandimmune), tacrolimus (Prograf) and sirolimus (Rapamune)
- Amiodarone (Cordarone)
- Sildenafil (Viagra)
Herbal and Prescription Medicine Interactions
Herbal Products and Prescription Medicine shows combinations of herbal products and prescription drugs and the medical problems that could result.
If you take these combinations, this could happen:
Aloe + digoxin heart medicine: Lowers potassium in the blood
Aloe + steroids or blood pressure medicine: Lowers potassium in the blood
Cats Claw + blood pressure medicine: Dangerously low blood pressure
Cats Claw + immunosuppressants: Immunosuppressant doesn’t work well
Chondroitin + blood-thinners: Risk of bleeding
Echinacea + immunosuppressants: Immunosuppressant doesn’t work well
Fish oil capsules + blood thinners: Risk of bleeding
Garlic pills + blood-thinners, aspirin: Risk of bleeding
Garlic pills + Diabetes medicine: Dangerously low blood sugar
Garlic pills + cyclosporine: Organ rejection
Gingko Biloba + blood-thinners: Risk of bleeding
Gingko + diuretic blood pressure pills: Higher blood pressure
Gingko + anticonvulsants: Risk of seizures
Ginseng + blood-thinners: Risk of bleeding
Glucosamine + Diabetes medicine: May raise blood sugar
Glucosamine + cancer medicine: Cancer medicine doesn’t work well
Hawthorn + digoxin heart medicine: Irregular heartbeat
St. John’s Wort + Digoxin: Digoxin doesn’t work well
St. John’s Wort + psychiatric medicine: Toxic side effects
St. John’s Wort + Cyclosporine: Organ rejection
St. John’s Wort + blood thinners: Blood thinners don't work well
Resources for more information about medicine interactions
There are many, many more interactions than can be listed here. Get in the habit of asking your pharmacist or physician before starting a new OTC product. Or you can look on-line at reputable medical websites such as WebMD or https://nccam.nih.gov/health/.
Tennessee Poison Center (1-800-222-1222) is a free source of information just a phone call away. Nurses, pharmacists and physicians answer questions on the hotline 24 hours a day. If someone feels unwell after mixing medications, Tennessee Poison Center can help in a matter of minutes. In most cases, the caller can be taken care of in their own home while following the poison centers advice. The statewide toll-free Poison Help hotline number is 1-800-222-1222.
* Reprinted original article by JoAnn Chambers-Emerson, RN, BSN, CSPI Certified Specialist in Poison Information Florida Poison Information Center Tampa
-
IF YOU TAKE THESE: THIS COULD HAPPEN: Aloe & digoxin heart medicine
Aloe & diabetes medications
Aloe & diuretics (water pills)
Beta-Carotene & cigarette smoking
Beta-Carotene & cigarette smoking
Capsicum & blood-thinner medicines
Cat's Claw & blood pressure medicines
Cat's Claw & immunosuppressants
Chondroitin & blood thinner medicines
Echinacea & immunosuppressants
Ephedra & digoxin heart medicine
Ephedra & diabetes medicine
Fish oils & blood thinner medicines
Garlic pills & blood thinner medicines, aspirin
Garlic pills & diabetes medicines
Garlic pills & cyclosporine/HIV medicines
Gingko Biloba & blood thinner medicines
Gingko Biloba & anticonvulsants (seizures)
Ginseng & blood thinner medicines
Ginseng & diabetes medicines
Glucosamine & some cancer medicines
Glucosamine & shellfish allergy
Hawthorn & digoxin heart medicine
Kava-kava if you have liver problems
St. John's Wort & digoxin heart medicine
St. John's Wort & psychiatric medicines
St. John's Wort & cyclosporine
St. John's Wort & blood thinner medicines
St. John's Wort & certain migraine medicinesLow potassium levels
Low blood sugar levels
Low potassium levels
Higher cancer risk
Higher heart attack risk
Risk of bleeding
Low blood pressure
Reduced effectiveness of medicine
Risk of bleeding
Reduced effectiveness of medicine
Irregular heart beat
High blood sugar levels
Risk of bleeding
Risk of bleeding
Lower blood sugar levels
Reduced effectiveness of medicine
Risk of bleeding
Risk of seizures
Risk of bleeding
Risk of low blood sugar levels
Reduced effectiveness of medicine
Allergic reaction
Irregular heart beat
Severe liver damage
Reduced effectiveness of digoxin
Risk of toxic side effects
Reduced effectiveness of medicine
Reduced effectiveness of medicine
Risk of toxic side effectsPOTENTIAL GRAPEFRUIT & GRAPEFRUIT JUICE MEDICINE INTERACTIONS
If you take any of the following medicines, please be sure and ask your physician or pharmacist for the most current information before eating grapefruit or drinking grapefruit juice:
- Medicines used to treat high blood pressure
- Medicines used to treat/lower cholesterol levels, such as "statin" medicines
- Medicines used to treat anxiety, such as "anti-anxiety" medicines
- Medicines used to treat cold and cough symptoms, such as "antihistamine" medicines
- Medicines used to treat HIV/AIDS, such as "protease inhibitors" medicines
- Medicines used to treat/reduce organ rejection after transplant surgery, such as "immunosuppressants"
Want to learn more about medicine interactions? Visit the following websites:
https://www.webmd.com/interaction-checker/default.htm
This information is to be used for educational and informational purposes only. As always, speak with your physician about any questions you may have about your medicines and possible interactions. Call the Poison Help hotline if you have questions or experiencing symptoms from mixing medicines at 1-800-222-1222.
-
One Reason why you should read the label on medications:
Sound-a-likes
Clonidine, clozapine, Klonopin-same drugs? Different drugs?
The difficulty in medicine is that some drugs sound alike in their pronunciations just like the examples given. One of these medications may be used for blood pressure control, one may be used to treat patients who have schizophrenia and one may be used to treat seizures-very different drugs, very different actions. In the overdose setting, the effects are quite different as well.
If a patient or a physician calls the poison center about one of these medications, we may have them spell the name to make sure that we have the right name and are giving the correct information about the medication. For patients, you should understand why you are taking the medication and make sure you have the correct spelling. This reduces the risk of prescribing other medications that may interact with the one you are on. If your pharmacist doesn’t know what other medications you are taking, they won’t be able to best advise you about possible interactions or side effects.
Consider having a written medication list that spells out the medication and the dose so there is no mistaken about what you are actually taking.
Another reason why you should read the label on medications:
Misadventures with pediatric acetaminophen products
Acetaminophen is a commonly used medication to treat fevers and pain. Although it is mostly commonly known as Tylenol®, acetaminophen is in many products that are used for pain relief and cold medications.
One issue that parents need to know about is that not all children’s versions of acetaminophen-based products are created equal. Some of these products are a more concentrated version of the acetaminophen. For instance, the Infant concentrated drops, each dropperful provides 0.8 milliliters (0.8 mL) of liquid which contains 80 mg of acetaminophen. The advantage of this concentrated type of medicine is that less liquid is needed to provide a dose of medication to an infant.
The elixir acetaminophen product is usually dosed in teaspoons, instead of dropperfuls. A teaspoon contains 5 milliliters (5 mL) of liquid. A teaspoon of the elixir product contains 160 mg of acetaminophen. The elixir is less concentrated than the infant drops.
The problem occurs when someone is using the infant concentrated drops and giving a dose based on the elixir. For example, a child is supposed to have 160 mg of acetaminophen. This would mean 2 dropperfuls (1.6 mL) of the infant concentrated drops or one teaspoon (5mL) of the elixir. If someone mistakenly gives a teaspoon (5 mL) of the infant concentrated drops, then the child will receive a dose of 500 mg of acetaminophen rather than the right dose of 160 mg. This can result in an overdose of acetaminophen. Although acetaminophen is very safe when given in normal doses, an overdose may cause liver toxicity.
Always ask your pediatrician how much acetaminophen you should give your very young child and make sure you know which type of acetaminophen product you are using so that it can be given safely.
-
An EMR warning frequently occurs when prescribing concomitant drugs that have the potential to prolong the QT interval. This warning occurs when we are going to prescribe a single dose of fluconazole to treat yeast vaginitis as a patient is finishing a course of fluoroquinolone OR when the patient is on an SSRI. I think most clinicians override that warning but is it safe? Should we use more caution?
We received the above question from one of our favorite physicians and Question of the Week readers. Great question. So, I asked two experts: Nena Bowman, Pharm D, DABAT, Managing Director of TPC, and Dan Roden MD, Senior VP of personalized Medicine at VUMC and wizard of all things QT. ds
Nena said:
Information from drug databases which include drug interactions can be difficult to interpret. Their true utility comes from the information they so readily provide, but how that translates into clinical practice is a different animal altogether. I entered "fluconazole, fluoxetine, and ciprofloxacin" into Micromedex drug interactions which displayed an interaction risk of "major”. With an interaction warning such as this, decisions should be based on level of evidence. For all three of these interactions, the level of evidence is "fair", which is defined by Micromedex as "Available documentation is poor, but pharmacologic considerations lead clinicians to suspect the interaction exists; or, documentation is good for a pharmacologically similar drug."
Therefore while all three drugs independently carry some risk for QT prolongation, the potential for the combination of the drugs to prolong QT is theoretical, and the clinical decision comes down to risk / benefit. If the drugs have blackbox warnings for QT prolongation, an EKG can rule out baseline prolonged QT before adding the third drug. I would not recommend starting three new drugs - all that carry risk for QT prolongation - at the same time.
It all comes down to risk / benefit and the level of evidence. A risk category of "major" means that the possible effect could be life-threatening IF it occurs - NOT that it is likely to occur.Dan said;
Hard to get excited about a single dose. The fluoroquinolone scenario doesn’t disturb me at all. The chronic SSRI scenario could get a bump in plasma levels from one dose, but the likelihood that a bump would be big enough to dramatically prolong QT seems far-fetched unless the QT in the SSRI is very long to start with.
So, there you have it. One final thought- Remember that drug-induced torsades almost always occurs in the setting of bradycardia. And congratulations to Dr. Roden for winning the Schotenstein Prize that honors leaders in CV sciences who have made extraordinary and sustained contributions to improving healthcare. Congratulations also to Dr. Bowman who has just been elected President of the Nashville Area Pharmacists Association (NAPA). ds
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vumc.org.
Donna Seger, MD
Executive Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
-
Toxicology Question of the Week
02/03/2020
When Does Ondansetron Prolong the QT Interval?
A common question we address in the Poison Center is if QT interval prolongation is a concern when ondansetron is administered. A 2012 safety announcement by the FDA warned healthcare professionals that administration of ondansetron could cause QT prolongation and potentially Torsades de Pointes (TdP). This announcement was based on preliminary results from a clinical study regarding an intravenous 32mg single dose of ondansetron. The FDA announcement stated, “The lower dose intravenous regimen of 0.15 mg/kg every 4 hours for three doses may be used in adults with chemotherapy-induced nausea and vomiting. However, no single intravenous dose of ondansetron should exceed 16 mg due to the risk of QT prolongation.” The announcement also stated, “the new information does not change any of the recommended oral dosing regimens for ondansetron, including the single oral dose of 24 mg for chemotherapy induced nausea and vomiting.”
Oral ondansetron should not prolong the QT interval. High dose IV ondansetron is the only scenario that increases risk for QT prolongation and TdP. If you have any questions / concerns, contact the Tennessee Poison Center!
Prepared by: Diana Hakim, Lipscomb University College of Pharmacy, PharmD Candidate 2020: Nena Bowman, PharmD, DABAT, Managing Director of TPC.
Reference:
As with many drugs, the intravenous administration (which bypasses hepatic metabolism and causes higher serum drug concentrations) can cause different effects compared to oral administration. When FDA warnings are released, methods of administration are sometimes overlooked, and the assumption is that any administration can cause the effect discussed in the warning. BTW, remember that the FDA is a committee-a consensus committee. -ds
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vumc.org.
Donna Seger, MD
Executive Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
-
Toxicology Question of the Week
April 10, 2019
What is LUCEMYRA®?
What is it?
Lucemyra® (lofexidine hydrochloride): 2-(1-)2,6-dichlorophenoxy(ethyl)-2-imidazoline) was recently FDA approved for the mitigation of withdrawal symptoms to facilitate abrupt discontinuation of opioids in adults. It is the first FDA approved non-opioid treatment for the management of opioid withdrawal symptoms.
How does it work?
Lofexidine is an oral, central alpha 2-adrenergic receptor agonist that reduces the release of norepinephrine and decreases sympathetic tone. Lofexidine binds to alpha-2A and alpha-2C adrenoreceptors, and due to its high selectivity for the alpha-2A receptors, it is thought to have less potent anti-hypertensive effects than clonidine. The actions of norepinephrine in the autonomic nervous system are believed to play a role in many of the symptoms of opioid withdrawal.
What is the current treatment for Opioid withdrawal?
Opioid withdrawal symptoms include anxiety, agitation, sleep problems, muscle aches, runny nose, sweating, nausea, vomiting, diarrhea and drug craving. Opioid withdrawal is typically managed by slowly tapering opioids followed by maintenance therapy with an FDA approved medication-assisted treatment drug such as methadone, buprenorphine or naltrexone or by various medications aimed at specific symptoms. Lofexidine is the first FDA approved non-opioid drug for the treatment of opioid withdrawal symptoms.
What are the adverse effects and drug handling considerations?
- Cardiovascular effects: bradycardia, hypotension and QT prolongation
- CNS effects: drowsiness, dizziness, insomnia
- Gastrointestinal: dry mouth
- Lofexidine may cause teratogenicity and reproductive toxicity
- Use with precautions for receiving, handling, administration, and disposal Gloves (single) should be worn during receiving, unpacking, and placing in storage
Conclusion:
When Lofexidine is stopped, patients can experience a marked increase in blood pressure. The safety and efficacy of Lofexidine have not been established in children or adolescents less than 17 years of age. Clinical studies will be required to evaluate the safety of Lofexidine in clinical situations where use could be expected to exceed the maximum 14-day treatment period for which the product is currently approved.
References:
http://online.lexi.com/lco/action/doc/retrieve/docid/patch_f/4854487#cpg
https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/209229s000lbl.pdf
https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm607884.htm
This question was prepared by: Suparna Kumar MD, CSPI
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vumc.org.
Donna Seger, MD
Executive Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
-
Toxicology Question of the Week
April 1, 2019
What is PRIS, what are markers of severity, and how is the syndrome treated?
Propofol is one of the most commonly used intravenous anesthetic agents used in ICU and OR settings. Propofol infusion syndrome (PRIS) is a term that describes a rare clinical syndrome that was first described in the 1990s through case reports where patients suffered cardiovascular collapse in the setting of prolonged and high-dose propofol infusions. While the definition of PRIS is controversial due to its rarity and poorly understood etiology, it is generally defined as a “relatively sudden onset of metabolic acidosis, with cardiac dysfunction, and at least one of the following findings: rhabdomyolysis, hypertriglyceridemia, and renal failure.” Early cardiac findings can include bradycardia and RBBB (1). After initial case reports described the syndrome, additional research in the form of retrospective analyses was conducted to further characterize the clinical syndrome. While initially thought to be a syndrome that only occurs in pediatric patients, it has been described in adult patients as well.
The mechanism of PRIS remains unclear at this point; theories have been proposed about the cause being related to impaired hepatic lactate metabolism, and impaired mitochondrial respiratory chain function. A 2018 in vitro study published in PLOS One demonstrates various metabolic and biochemical including mitochondrial apoptotic pathway, results in increased ROS and decreased mitochondrial complex activity when cells are exposed to clinically relevant concentrations of propofol. Authors also proposed a metabolic switch phenomenon from oxidative phosphorylation to glycolysis that could contribute to the lactic acidosis that is seen in PRIS (2)
The common end-point in cases of PRIS is myocardial failure and cardiovascular collapse. (3) Common findings associated with PRIS include bradycardia/asystole, metabolic acidosis, hyperkalemia, rhabdomyolysis, myoglobinuria, and hepatomegaly. A diagnosis of PRIS should be considered when this constellation of signs occur at any point with concurrent use of propofol, but especially in the setting of prolonged (>48hr) and high dose (>4mg/kg/hr) infusions have been used. (2)
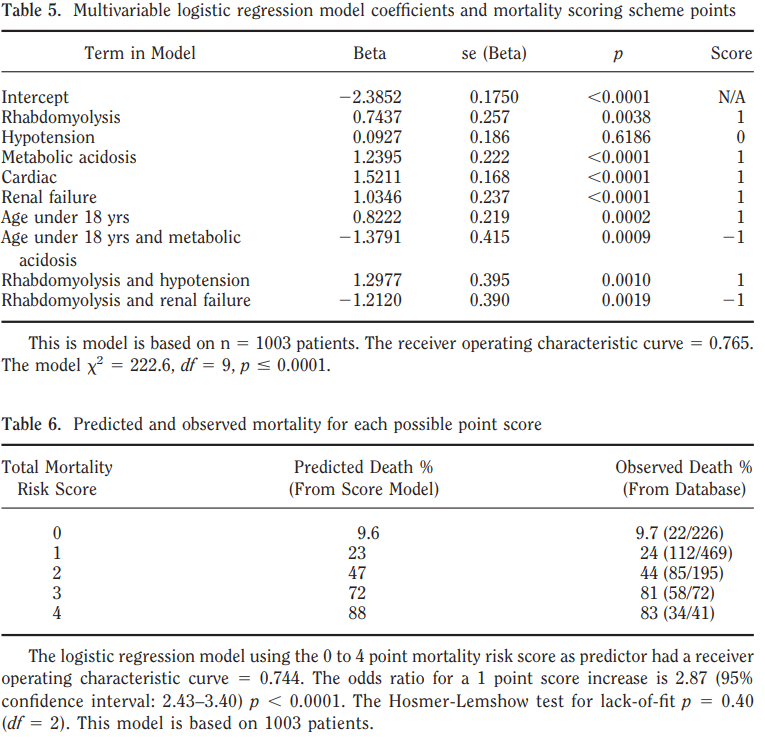
A 2008 study in Critical Care Medicine (4) used a multivariate logistic regression model to create a point-scoring scheme to predict mortality based on clinical features. Factors that were associated with increased risk of mortality include rhabdomyolysis, cardiac involvement, metabolic acidosis, renal failure, and hypotension. See the tables below for regression model coefficients and mortality scoring scheme.
- Pardo, Manuel, and Ronald D. Miller. Basics of Anesthesia. Elsevier, 2018.
- Sumi C, Okamoto A, Tanaka H, Nishi K, Kusunoki M, Shoji T, Uba T, Matsuo Y, Adachi T, Hayashi JI, Takenaga K, Hirota K. Propofol induces a metabolic switch to glycolysis and cell death in a mitochondrial electron transport chain-dependent manner. PLoS One. 2018 Feb 15;13(2):e0192796. doi: 10.1371/journal.pone.0192796. eCollection 2018. PubMed PMID: 29447230; PubMed Central PMCID: PMC5813975.
- Kam PC, Cardone D. Propofol infusion syndrome. Anaesthesia. 2007 Jul;62(7):690-701. Review. PubMed PMID: 17567345.
- Fong JJ, Sylvia L, Ruthazer R, Schumaker G, Kcomt M, Devlin JW. Predictors of mortality in patients with suspected propofol infusion syndrome. Crit Care Med. 2008 Aug;36(8):2281-7. doi: 10.1097/CCM.0b013e318180c1eb. PubMed PMID: 18664783.
This question was prepared by: Brett Shaffer, MD PGY-4 Anesthesiology Resident
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vumc.org.
Donna Seger, MD
Executive Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
The Question of the Week is available on our website: www.tnpoisoncenter.org
-
Toxicology Question of the Week
March 27, 2019
Why do we give glucagon in beta blocker overdose?
Beta blockers competitively inhibit myocardial β1 receptors. These receptors normally act through a second messenger system (Gs proteins*) to activate adenyl cyclase (AC) and increase cyclic AMP (cAMP), which results in the influx of intracellular calcium through L-type calcium channels. β1-receptor antagonism results in decreased calcium entry and, subsequently, decreased inotropy and chronotropy.
Glucagon, a polypeptide counterregulatory hormone secreted from the pancreatic α-cells, bypasses β-receptors to exert inotropic and chonotropic cardiac effects. Similar to β-receptors, cardiac glucagon receptors are coupled to Gs proteins. Glucagon binding to these receptors results in increased adenylyl cyclase activity independent of β-receptor activity.
We recommend giving glucagon as a 10 mg bolus over 10 minutes. Giving the bolus more quickly increases risk for vomiting. Glucagon has a short half-life and the bolus should be followed by a continuous infusion at 3-5 mg/hr.
Glucagon may also be considered in other cases of drug-induced bradycardia.
References
DeWitt, C.R. and J. C. Waksman (2004). "Pharmacology, pathophysiology and management of calcium channel blocker and beta-blocker toxicity." Toxicol Rev 23(4): 223-238.
Graudins, A., et al. (2016). "Calcium channel antagonist and beta-blocker overdose: antidotes and adjunct therapies." Br J Clin Pharmacol 81(3): 453-461.
Nelson, L.S., Lewin N.A., Howland, M.A. (Eds.), et al. Goldfrank's toxicologic emergencies 9th edition (McGraw-Hill Education, New York, 2011).
Shepherd, G. (2006). "Treatment of poisoning caused by beta-adrenergic and calcium-channel blockers." Am J Health Syst Pharm 63(19): 1828-1835.
This question prepared by: Cosby Arnold MD, UT Emergency Medicine Resident
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vumc.org
Donna Seger, MD
Executive Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
-
Toxicology Question of the Week
January 17, 2019
What are the concerns with ADHD medications?
Medications used to treat Attention Deficit Hyperactivity Disorder (ADHD) fall into two categories:
- Stimulants: amphetamine salts, lisdexamphetamine, methylphenidate
- Non-Stimulants: atomoxetine, clonidine, guanfacine
Amphetamines and methylphenidate act to inhibit the cellular reuptake of dopamine and less so norepinephrine and serotonin. Toxicity is due to excessive extracellular dopamine, norepinephrine, and serotonin, though methylphenidate also directly activates dopamine-1 receptors on postsynaptic neurons. Lisdexamphetamine (Vyvanse) is a prodrug that is cleaved to release the active dextroamphetamine by red blood cell hydrolysis; this rate-limiting step of activation may produce a delay in symptom onset by several hours. The most prominent clinical presentation is alpha- and beta-adrenergic receptor-mediated sympathomimetic syndrome, with psychiatric symptoms and hyperthermia secondary to dopamine and serotonin excess.
In overdose, the patient may present with anxiety, paranoia, insomnia, agitation, confusion, delirium, hallucinations, tremor, hyperreflexia, movement disorders, tachycardia, hypertension, dysrhythmias, hyperthermia, and seizures. Sedation may occur secondary to catecholamine depletion, post-ictal state, ischemic stroke, or intracerebral hemorrhage. Rhabdomyolysis may occur due to psychomotor agitation, hyperthermia, or seizures. Late-state refractory hypotension may occur with seizures, hyperthermia dysrhythmias, and acidosis.
The management of stimulant overdose is largely supportive with a focus on the cessation of the sympathomimetic syndrome. Intravenous benzodiazepines are first-line agents. Doses should be titrated to clinical response (large doses may be required). If intravenous access cannot be obtained due to combative behavior, intramuscular administration of benzodiazepines or ketamine is recommended until intravenous access can be established. Hyperthermia should be treated with external cooling. Hypertension and tachycardia typically respond to adequate sedation.
Atomoxetine is a selective norepinephrine reuptake inhibitor with no reported effects on dopamine or serotonin. Toxicity is related to excessive extracellular norepinephrine. Reports of overdose have generally been mild. Patients typically experience drowsiness (primarily pediatrics), agitation, tremor, hyperreflexia, hypertension, sinus tachycardia, and seizure. Treatment follows that of stimulants.
Clonidine and guanfacine are agonists at both central alpha-2 and peripheral alpha-1 adrenergic receptors with some activity on imidazoline receptors as well. Activation of receptors in the locus coeruleus produces miosis and CNS/respiratory depression similar to that of opioid intoxication, while activation of receptors in the medulla decreases norepinephrine release which results in decreased heart rate, cardiac output, and peripheral vascular resistance. Initial paradoxical hypertension and vasoconstriction may occur due to stimulation of peripheral alpha-1 adrenergic receptors, but this is usually transient as the potent central sympatholytic effects quickly dominate.
The management of clonidine/guanfacine overdose is largely supportive with a focus on adequate ventilation and the support of blood pressure. High-dose naloxone (10 mg) may reverse the hypotension and somnolence. If it is effective, then initiate a 5mg/hour drip and titrate to clinical response. Otherwise, treatment should follow standard supportive care. Sinus bradycardia without hypotension or symptoms of hypoperfusion does not require intervention. Patients with severe bradycardia and hypotension unresponsive to high-dose naloxone may benefit from dopamine or norepinephrine.
This question prepared by: Justin Loden, PharmD, CSPI, DABAT
References
- Forrester MB. Pediatric atomoxetine ingestions reported to Texas poison control centers, 2003-2005. J Toxicol Environ Health A. 2007 Jun; 70(12):1064-70.
- Jang DH. Chapter 76: Amphetamines. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, editors. Goldfrank’s Toxicologic Emergencies, 10th ed. New York: McGraw-Hill; 2015. http://accesspharmacy.mhmedical.com/book.aspx?bookid=1163
- Kappagoda C, Schell DN, Hanson RM, et al. Clonidine overdose in childhood: implications of increased prescribing. J Pediatric Child Health. 1998 Dec; 34(6):508-12.
- Klein-Schwartz W. Trends and toxic effects from pediatric clonidine exposures. Arch Pediatr Adolesc Med. 2002 Apr; 156(4):392-6.
- Krishnan SM, Pennick M, Stark JG. Metabolism, distribution, and elimination of lisdexamfetamine dimesylate: open-label, single-center, phase I study in healthy adult volunteers. Clin Drug Investig. 2008; 28(12):745-55.
- LoVecchio F, Kashani J. Isolated atomoxetine (Strattera) ingestions commonly result in toxicity. J Emerg Med. 2006 Oct; 31(3):267-8.
- Seger DL. Clonidine toxicity revisited. Clin Toxicol (Phila). 2002; 40(2):145-55.
- Seger DL, Loden JK. Naloxone reversal of clonidine toxicity: dose, dose, dose. Clin Toxicol (Phila). 2018; 56(10):873-79.
- Spiller HA, Klein-Schwartz W, Colvin JM, et al. Toxic clonidine ingestion in children. J Pediatr. 2005 Feb; 146(2):263-6.
- Spiller HA, Lintner CP, Winter ML. Atomoxetine ingestions in children: a report from poison centers. Ann Pharmacother. 2005 Jun; 39(6):1045-8.
Westfall TC, Westfall DP. Chapter 12: Adrenergic Agonists and Antagonists. In: Brunton LL, Chabner BA, Knollman BC, editors. Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th ed. New York: McGraw-Hill; 2011. http://accesspharmacy.mhmedi
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vanderbilt.edu
Donna Seger, MD
Executive Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
The Question of the Week is available on our website: www.tnpoisoncenter.org
-
Toxicology Question of the Week
March 26, 2018
Does naloxone reverse clonidine toxicity?
The issue of administering hi-dose naloxone to pediatric patients has caused more anxiety than you can imagine. I have had many calls from physicians when the Poison Center recommends administering 10 mg naloxone IVP to children. Pharmacists have refused to fill the order, nurses have refused to administer it, and I have even received a call from a Chief of Staff regarding our recommendations. This is not a mg/kg dose/response. We are trying to reverse released endorphins, which require the same amount of naloxone, no matter how big you are. Now we have demonstrated that hi-dose naloxone in clonidine toxicity is safe and that it works the majority of the time.
Naloxone reverses toxicity because clonidine causes the release of beta-endorphin (in patients with higher sympathetic tone) and naloxone reverses the effects of the beta endorphin. However large doses are required. Administering 2 mg five times is not the same as administering 10 mg IVP. AND, it doesn’t work as well in those with lower sympathetic tone (which we have no way of determining clinically).
When naloxone is not administered to children with clonidine toxicity, they get intubated- not an innocuous procedure. A toxicologist told me of the death of a 2 year-old following clonidine ingestion in a small ED in New England. The doctor was unable to intubate the child. Naloxone had not been administered.
As always, call the poison center with any questions regarding clonidine ingestions. There is always a medical toxicologist on call if you want to speak to a physician ds
The records of 52 patients seen by the Toxicology Consult Service and followed by the TN Poison Center were reviewed. High-dose naloxone awoke the majority (78.5%) of patients and resolved bradycardia and hypotension in some. Persistent bradycardia was benign, and hypotension was rare and clinically insignificant. No adverse reactions occurred in any patient who received naloxone. See the attached study.
This Question was prepared by: Justin Loden, PharmD, CSPI (Certified Specialist in Poison Information)
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vanderbilt.edu
Donna Seger, MD
Medical Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
The Question of the Week is available on our website: www.tnpoisoncenter.org
-
Toxicology Question of the Week
March 23, 2017
How does Metformin differ from other oral hypoglycemic drugs?
Metformin is a biguanide agent and the drug-of-choice for the treatment of newly diagnosed type-2 diabetes mellitus, making it one of the most widely prescribed medications in the world. With over half a century of clinical experience, metformin is generally recognized as safe with the most frequent adverse effects being gastrointestinal (i.e. nausea, indigestion, abdominal cramps/bloating, diarrhea). Metformin acts to reduce hepatic glucose production, reduce intestinal glucose absorption, and increase skeletal muscle glucose uptake and utilization. Because it does not affect the release of insulin or other pancreatic hormones, metformin is rarely associated with hypoglycemia.
Metformin impairs mitochondrial respiration and inhibits the conversion of lactate to pyruvate. This results in both an increased production and decreased elimination of lactate with a subsequent acidosis known as metformin-associated lactic acidosis (MALA). MALA is a serious but rare complication of metformin therapy (less than 10 events per 100,000 patient-years of exposure) with a mortality rate that approaches 50%. MALA as a result of therapeutic use is typically due to an acute event that affects the patient’s ability to excrete metformin (i.e. acute kidney injury) coupled with risk factors that increase lactate production and/or retention (see table below). Small changes in hydration, renal function, plasma metformin concentrations, and tissue oxygenation often lead into a positive feedback loop that worsens the lactic acidosis. Acute metformin overdose is the most frequent cause of MALA.
Table 1-1: Risk Factors that Increase
Lactate Production/Retention
Renal Insufficiency
Alcoholism (NAD+ depletion)
Liver Dysfunction
Sepsis
Surgery
Congestive Heart Failure
Hypoxemia
Advanced Age
Symptoms of MALA are nonspecific and include nausea, vomiting, abdominal pain, malaise, myalgia, and dizziness. More severe manifestations of the lactic acidosis include mental status depression, confusion, hypotension, hypothermia, and respiratory insufficiency. Serum metformin levels can be obtained as a diagnostic aid, but concentrations are not directly proportional to the severity of the lactic acidosis.
Patients with an acute overdose of immediate-release tablets require a 6-hour observation period and extended-release tablets a 12-hour observation period. Serum electrolytes and lactate should be checked every 2 hours to monitor for the development of metabolic acidosis or hyperlactatemia. Those who develop symptoms or laboratory abnormalities should be admitted for possible treatment.
The cornerstone of therapy for MALA is resuscitation and supportive care as there is no specific antidote available to reverse the toxic effects of metformin. Hemodialysis is indicated for severe toxicity in order to remove lactate, correct electrolyte abnormalities, and support impaired renal function. Sodium bicarbonate may need required to temporarily correct acidemia until hemodialysis is available, while intravenous fluids and inotropic agents should be used to improve cardiovascular function.
References
- Al-Abri SA, Hayashi S, Thoren KL, et al. Metformin overdose-induced hypoglycemia in the absence of other antidiabetic drugs. Clin Tox. 2013; 51(5):444-47.
- Calello DP, Liu KD, Wiegand TJ, et al. Extracorporeal treatment for metformin poisoning: systematic review and recommendations from the extracorporeal treatments in poisoning workgroup. Crit Care Med. 2015; 43:1716-30.
- DeFronzo R, Fleming GA, Chen K, et al. Metformin-associated lactic acidosis: current perspectives on causes and risk. Metabolism. 2016 Feb; 65(2):20-9.
- Duong JK, Furlong TJ, Roberts DM, et al. The role of metformin in metformin-associated lactic acidosis (MALA): case series and formulation of a model of pathogenesis. Drug Saf. 2013 Sep; 36(9):733-46.
- Lalau JD. Lactic acidosis induced by metformin: incidence, management, and prevention. Drug Saf. 2010 Sep; 33(9):727-40.
This question prepared by: Justin Loden, PharmD, CSPI (Certified Specialist in Poison Information)
-
Question of the Week
February 28, 2017
Why is it important to admit an asymptomatic patient with a bupropion overdose?
Bupropion (brand name: Wellbutrin and Zyban) is medication that is FDA-approved to treat depression, to prophylactically treat seasonal affective disorder and to aid in smoking cessation. Off-label uses for bupropion include ADHD and bipolar disorder.
Bupropion is in a category of its own from other antidepressants (the SSRIs, SNRIs and tricyclics) because its mechanism of action is a little different. Bupropion inhibits the reuptake of norepinephrine and dopamine. This indirectly increases serotonin levels and acts as a stimulant.
Because it is often prescribed and available in households, intentional overdose occurs. Patients may present with nausea/vomiting, tachycardia, tremors, agitation, and seizures. In very high doses, a wide complex tachycardia and hypotension can be seen. Patients may also have hallucinations, lethargy and confusion. Because of the indirect effect on serotonin, a patient could also present after an overdose with serotonin syndrome.
Bupropion is metabolized to three active metabolites, the majority to hydroxybupropion. Though bupropion reaches peak levels in the blood 2h after ingestion and has a half-life of 16h, the active metabolite is around longer and does not reach peak levels until all the bupropion is metabolized. This active metabolite is what causes seizures. As the active metabolite slowly increases, patients may seizure 12 to 18 hours after the initial ingestion of bupropion. This may be further delayed in any extended release preparations. Because of the length of time that the active metabolites are in the system, it is important to keep a close eye and seizure precautions on any bupropion overdose. The seizures are usually self-limited and can be treated with benzodiazepines. Benzodiazepines can also be used to treat any extreme agitation or tremors that may develop.
As an interesting aside, the structure of bupropion is similar to that of amphetamines and can cause a false positive on a urine drug screen.
This question prepared by: Kristy Morse, MD Pediatric Emergency Medicine Fellow LeBonheur Children’s Hospital
I am interested in any questions you would like answered in the Question of the Week. Please email me with any suggestion at donna.seger@vanderbilt.edu
Donna Seger, MD
Medical Director
Tennessee Poison Center
Poison Help Hotline: 1-800-222-1222
-
Question of the Week
February 14, 2017
There are a number of advertisements regarding Brain Boosters. Now you can get the real scoop. /ds
Should you take brain boosting supplements in 2017?
The New Year brings a sense of fresh motivation to make changes, experience new things, and improve health. Recently, a brain booster falsely advertised by a faux CNN copycat website touted improved critical thinking capabilities with the ability to access 100% of the human brain. It included faux endorsements by Anderson Cooper and Stephen Hawking, crediting the new supplement, BrainPlus IQ ® for their success and genius. Supplements and herbal complexes are not FDA regulated and can contain inconsistent amounts of active ingredients.
According to the product’s website, this product is a phosphatidylserine complex based nootropic. Typically this active ingredient is harvested from bovine brain tissue. After concern for mad cow prion transmission, several products have gone to vegetarian sources of phosphatidylserine such as soy or cabbage. Side effects can include insomnia, stomach upset, and potential risk for disease transmission. Toxicologically phosphatidylserine complexes interact with anticholinergic drugs and acetylcholinesterase inhibitors. Patients taking selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors, (SNRIs), and monoamine oxidase inhibitors (MAOIs) are at risk to develop effects associated with serotonin syndrome.
Cogniq® is also a popularly advertised nootropic brain booster. It contains phosphatidylserine complexes as well as other herbal supplements including St. John’s Wort, glutamate, ginkgo biloba, and dimethylaminoethanol. Ginkgo biloba can interact with blood thinners and increase risk of bleeding. St. John’s Wort can interact with SSRIs, SNRIs, and MAOIs, causing symptoms associated with serotonin syndrome; it also interacts with the metabolism and elimination of many medications, leading to increased risk of toxicity or accumulation of other medications.
The Tennessee Poison Center was recently contacted about a therapeutic error with the nootropic agent Addium® in an adult female. The patient’s home medications included atorvastatin and escitalopram. She was calling initially complaining of facial flushing and extremity flushing and redness. Symptoms resolved in two hours post ingestion without any interventions. The active ingredients of this product are listed on the product website including L-Tyrosine, GABA, bacopa monnieri, Alpha GPC, vinpocetine, and Huperzine A. These are all herbal supplements that are not FDA regulated and have been reported to cause symptoms such as flushing, sweating, nausea, vomiting, and diarrhea.
Often these products are marketed to elderly people who typically take chronic medications. Caution should be exercised when considering the initiation of a supplemental product while taking prescription medications. Please consult a physician or the Tennessee Poison Center with questions regarding exposures or drug interactions from these nootropic medications.
Product Websites:
http://brain-plus-iq.info/ingredients/
https://buycogniq.com/difference.php
This question prepared by: Nena Bowman, PharmD, CSPI (Certified Specialist in Poison Information) Tennessee Poison Center
-
Question of the Week
February 10, 2014
What is the clinical picture of Neuroleptic Malignant syndrome?
One of the consults that we receive is the question as to whether a patient has neuroleptic malignant syndrome (NMS). I had a recent case where an adolescent female overdosed on a SSRI. It led to a very informative discussion between the pediatric hospitalist and their pediatric resident team, psychiatry and toxicology. I thought it might be worthwhile to review some of the concepts that were discussed.
Although pathophysiologic mechanism is undetermined, some type of drug-induced dopamine blockade probably occurs.
No clinical signs and symptoms verify the diagnosis of NMS. An international panel has published a consensus paper on the diagnostic criteria required for the diagnosis of NMS-criteria which they note has not been validated. (J Clin Psychiatry 2010).
Here is my synopsis on NMS:
“Cardinal Symptoms” of NMS are 1)hyperthermia 2)lead-pipe rigidity 3)autonomic instability 4)altered mental status and 5)elevated CPK
1) Hyperthermia (may be delayed-usually associated with diaphoresis). Originally one of the clinical signs for the basis of the diagnosis, NMS was thought to be related to malignant hyperthermia because the temperature was so markedly elevated (102-107F). However now there are case reports of NMS with minimal temperature elevation. On a toxicology blog, an Australian toxicologist asks-If a patient has classic signs/symptoms of NMS but no hyperthermia, is it NMS?
2) Rigidity-lead pipe-the patient is so rigid that they have no reflexes or bradyreflexia. The extremities can be moved/molded into position, but stiffly.
3) Autonomic instability is defined as variability of >30 mm Hg systolic or >20 mg Hg diastolic between readings. Clinically, this is very impressive. As one stands at the bedside, every blood pressure and heart rate reading is different.
-Tachycardia is part of the autonomic dysfunction but is not part of the autonomic instability.
-Both hypo and hypertension occur
4) AMS-stupor, alert, mutism, coma
5) Elevated CPK (usually in the thousands) which reflects the underlying rhabdomyolysis
Frequent signs include diaphoresis, and sialorrhea (nurses complain of needing to change the sheets as the diaphoresis is massive. The patients that I have seen with NMS are sweating profusely)
Lab in NMS-In addition to increased CPK, white count is also increased, usually not >20,000
This is quite different than the clinical picture of Serotonin Syndrome (SS) where the patient is usually agitated and diaphoretic, deep tendon reflexes are increased (lower>upper) and clonus is present (different than lead pipe rigidity), temperature and CPK are not so high, and tachycardia does not include the autonomic instability. However, there are spectrums of both NMS and SS and it is always easier to describe the differences than make the clinical diagnosis.
Treatment is primarily supportive. Morbidity and mortality are much improved now as compared to a few years ago due to advances in supportive care.
Intravenous benzodiazepines are a great way to go rather than the intermittent boluses in which patient’s level of consciousness tends to go up and down. 2 mg midazolam/hour will keep most everyone happy.
This question prepared by: Donna Seger, MD Medical Toxicologist
-
Question of the Week
March 26, 2012
Why are prescription drugs so available?
12,000 US residents die annually from unintended prescription drug overdose. The US contains 4.6% of world population yet consumes 80% of the global hydrocodone supply. The US rate of prescription drug use is 11.3 prescriptions per person. In Tennessee, there are 17.3 prescriptions per person. As this is an average, many persons have more than the average to balance those who have fewer than this amount.
In the late 90s, the consensus of professionals was that chronic pain was being undertreated in individuals with impairment. These beliefs lead to liberalization of laws governing opioid prescriptions. And in 2000, JCAHO introduced new, more liberal pain management standards.
Diversion (channeling from legal sources to illicit marketplace) occurs from illegal sale and recycling of prescriptions by physicians and pharmacists; doctor shopping; theft, forgery or alteration of a prescription by patients; shorting (undercounting); pilferage by pharmacists/employees; medicine cabinet thefts and internet sales.
There is the erroneous belief that OTC medications or those prescribed by a physician are safe. This belief and easy availability has changed the face of teenage drug abuse. “You can always find a doctor who you can convince that you have a sleeping problem to get Ambien or that you have ADD and get Adderall. I have friends who have ailments who get lots of pills and sell them for cheap. As long as prescription drugs are taken right, they’re much safer than street drugs”. Pharming parties (prescription drugs are exchanged and randomly ingested) are very popular in many Tennessee communities.
This question prepared by: Donna Seger, MD Medical Toxicologist
-
Question of the Week
March 14, 2011
Are there any new issues with acetaminophen and prescription products?
On January 13, 2011, the FDA announced a rule change asking manufacturers to limit the amount of acetaminophen in prescription drug products to 325 mg per dosage unit (tablet, capsule, etc). Currently, many prescription pain medications contain 500 mg of acetaminophen per dosage unit. In addition, the FDA added a “black box warning” to these combination prescription medications with the potential to cause severe liver injury. These actions attempt to reduce the risk of severe liver injury associated with acute and chronic acetaminophen poisoning. Changes in formulation are to take effect within three years. Any products that remain on the market with more than 500 mg of acetaminophen after 3 years will then be dealt with in a regulatory manner by FDA.
In Tennessee, the most common drug exposure that causes death is acetaminophen alone or acetaminophen in combination with other products. This is also true nationally. Hepatotoxicity may occur with an acute ingestion as well as with chronic supratherapeutic ingestion. Chronic supratherapeutic ingestion occurs when someone ingests an over the counter (OTC) preparation (which may contain up to 500 mg of acetaminophen per dosage unit) and then ingests additional prescription pain medication which also contains 500 mg per dosage unit. Over the counter preparations are not affected by this new dosage rule.
As always, we recommend caution and a careful history including the number of acetaminophen containing products (OTC or prescription) to assess the total daily dose. Remember that maximal daily dose for an adult is 4 grams per day. The total amount for children is lower depending on their weight.
If you have questions about the management of a patient who has exceeded these dosing recommendations, please call us.
A listing of affected products can be found at http://www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm239874.htm.
This question prepared by: John G. Benitez, MD, MPH Medical Toxicologist
-
Question of the Week
February 7, 2011
How does pyridoxine work as the antidote for INH poisoning?
Isoniazid (INH) is used for the treatment of active and latent tuberculosis because of its interaction with mycobacterial enzymes; however, INH also creates a net deficiency of pyridoxine. INH and its metabolites bind to pyridoxine and pyridoxal 5’ phosphate (the activated form) and enhance their renal elimination. One of the metabolites of INH also inhibits the enzyme which converts pyridoxine to its active form. Pyridoxine’s activated form, pyridoxal 5’ phosphate, is the cofactor needed for production of GABA, an inhibitory neuron in the brain. GABA is actually created from glutamic acid which is one of the most excitatory neurotransmitters in the brain. With an INH overdose, there is less GABA and more excitatory glutamic acid. Convulsions occur and do not cease with administration of typical anticonvulsant therapies, most of which rely on GABA being present in order for them to work. Treatment with high dose pyridoxine will stop the convulsions.
Once adequate dosing of the pyridoxine is given, additional anticonvulsant therapy is not needed; however, many patients remain sedated from the dosage of benzodiazepines they received.
This question prepared by: Saralyn Williams, MD Medical Toxicologist
-
Question of the Week
February 15, 2010
What is HIE therapy?
HIE or Hyperinsulinemia-Euglycemia therapy is a relatively novel way of treating cases of severe calcium channel blocker (CCB) poisoning. HIE is variously known as HIET (hyperinsulinemia-euglycemia therapy), HDIT (high dose insulin therapy), and occasionally other acronyms.
The typical clinical pattern of a CCB overdose includes profound hypotension and bradycardia (usually a junctional rhythm). These clinical findings result from peripheral vasodilatation, poor contractility, and decreased cardiac conduction. Additional signs and symptoms include mental status deterioration, seizures, metabolic acidosis and hyperglycemia. The release of insulin from the beta islet cells in the pancreas is inhibited by CCB’s as insulin release is calcium channel mediated; thus hyperglycemia occurs. The degree of hyperglycemia predicts the probability of a severe poisoning (defined in one study as needing vasopressors or a pacemaker or resulting in death).
Cardiomyocytes manifest resistance to insulin in the CCB OD setting and have less available substrate for metabolism due to shock and hypoperfusion. Lactate accumulation occurs.
Studies demonstrate a dose response for insulin increasing contractility through Ca dependent and independent pathways in the myocyte. In addition, insulin increases the sensitivity of myocytes to a given level of intracellular calcium. Insulin also increases the number of glucose transporters in the myocyte so that glucose utilization is maximized. In the setting of CCB OD, intravenous insulin reverses the impairment of these pathways. There may be other beneficial pathways through which insulin may reverse the effects of CCB OD. Insulin therapy has also been utilized with beta-blocker poisoning which is resistant to conventional therapy.
What is the typical dose of insulin needed? Although there are no current studies specifically addressing this issue, multiple case reports and case series describe use of regular dose insulin and high dose insulin with improvement in the cardiovascular parameters of the patient. High dose insulin is defined as a bolus of 0.5-1 Unit/kg, followed by a drip with a rate of 0.5-1 Unit/kg/hr. Yes, you read this right, a dose of approximately 5-10 times that of normal! The infusion is titrated to maintain an appropriate blood pressure. Heart rate does not change with this therapy. With high dose insulin therapy, the blood glucose needs to be monitored closely. While a patient is hyperglycemic (>300 mg/dL), supplemental glucose is not needed, however as blood glucose reaches 250 mg/dL, supplemental glucose (D10) may be required to reduce the likelihood of hypoglycemia.
Question prepared by: John Benitez, MD, MPH Medical Toxicologist