Understanding Long COVID: An Unexpected Consequence of the Pandemic
On March 11, 2020, the World Health Organization declared the 2019 Novel Coronavirus (COVID-19) outbreak a pandemic. Despite the immense research into treatments and measures to stop the spread of infection, we’re still learning more about the effects of COVID-19 infections. Just four years since the start of the pandemic, we are faced with an unexpected byproduct of COVID-19 infection – Long COVID.
What is Long COVID?
Long COVID refers to the condition where symptoms of COVID-19 persist after the initial infection. The World Health Organization defines Long COVID as the “continuation or development of new symptoms three months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least two months with no other explanation.”
Around 65 million people globally and around 1 in 5 adults in the US are estimated to experience Long COVID. However, that number could be much larger due to undiagnosed cases and poor reporting practices in underserved communities.
Long COVID symptoms may not always be the same as COVID-19 symptoms. Long COVID also encapsulates any new symptoms that may appear, as well as any that may relapse or return. For example, that cough and shortness of breath that went away for a while and is back a month later.
You may think you have been infected with COVID-19 again. While this may be true since multiple reinfections are possible as the virus continues to mutate, another likely culprit is Long COVID
Risk factors for Long COVID
The greatest risk factor (and prerequisite) for developing Long COVID is getting COVID-19. However, not everyone who had a previous COVID-19 diagnosis will develop Long COVID.
In the United States, more than 15 million people have experienced Long COVID, and several studies from 2022 up until now have highlighted several key risk factors that lead to a higher chance of Long COVID. These risk factors include type 2 diabetes, hypertension, chronic lung disease, obesity, and depression.
Those who had a more severe case of COVID-19 that required a hospital stay, along with those already experiencing respiratory problems such as asthma before the initial infection, are also at a greater risk.
Long COVID and Brain Fog
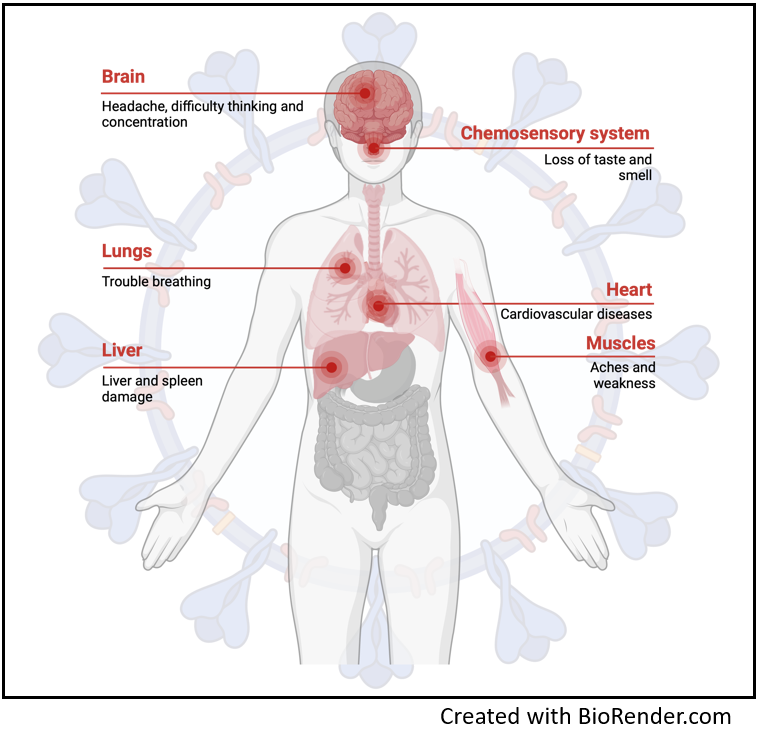
Just like COVID-19, symptoms of Long COVID vary from person to person and can range from mild to aggressive, hindering normal everyday activities. Symptoms generally include fatigue, muscle aches, loss of smell/taste, and shortness of breath. While these are the most common, there have been over 200 different symptoms reported.
One of the more common, and often described as the most debilitating, is brain fog. Brain fog is the decline in a person's ability to focus for extended periods. Brain fog can also include forgetfulness, confusion, always feeling tired or sluggish, and difficulty thinking. According to the American Medical Association, most Long COVID patients describe brain fog as feeling like their brain is lost in a maze and can't find a way back.
According to a study done in Central Texas, about 89% of patients from the study experienced brain fog and 46% had mild cognitive impairments. However, much is still unknown about exactly how COVID-19 infection and Long COVID are responsible for brain fog.
Efforts to determine this link between Long COVID and brain fog have been the focus of many studies published in the last few years. One study published in the Journal of Neuroinflammation showed that brain fog and COVID-related cognitive decline could be attributed to the virus’ ability to cross the blood-brain barrier and infect brain cells. This was done in vitro (meaning in test tubes), however, and has yet to be confirmed in animal or human studies.
Current Long COVID research at Vanderbilt
Since the beginning of the pandemic, many institutions have opened dedicated research centers focused on creating treatments and vaccines for COVID-19. Vanderbilt is no exception. Vanderbilt University Medical Center recently teamed up with scientists from several institutions across the US to launch a new clinical trial aimed at treating Long COVID. This trial will be testing an already FDA-approved drug known as baricitinib, sold under the brand name Olumiant. Barticitinib was originally used to treat rheumatoid arthritis and alopecia areata, but it was also the first COVID-19 treatment to receive FDA approval.
An article published by VUMC News earlier this year highlighting the trial states, “The study will test the hypothesis that six months of baricitinib will improve neurocognitive and physical function in Long COVID. Five hundred patients aged 18 and older who have had thinking and memory problems for at least six months after a COVID-19 infection will be enrolled and participate for one year.”
Not only will this trial look at the effects baricitinib will have on memory and cognitive functions, but it will also evaluate the ability of patients to exercise and improve their cardiorespiratory health.
The hope is that this trial and others like it will provide long-lasting treatment for those suffering the effects of Long COIVD. For more information, resources, and other COVID-19 research happening at Vanderbilt, check out the Vanderbilt Office of Health and Wellness.

