Our Program
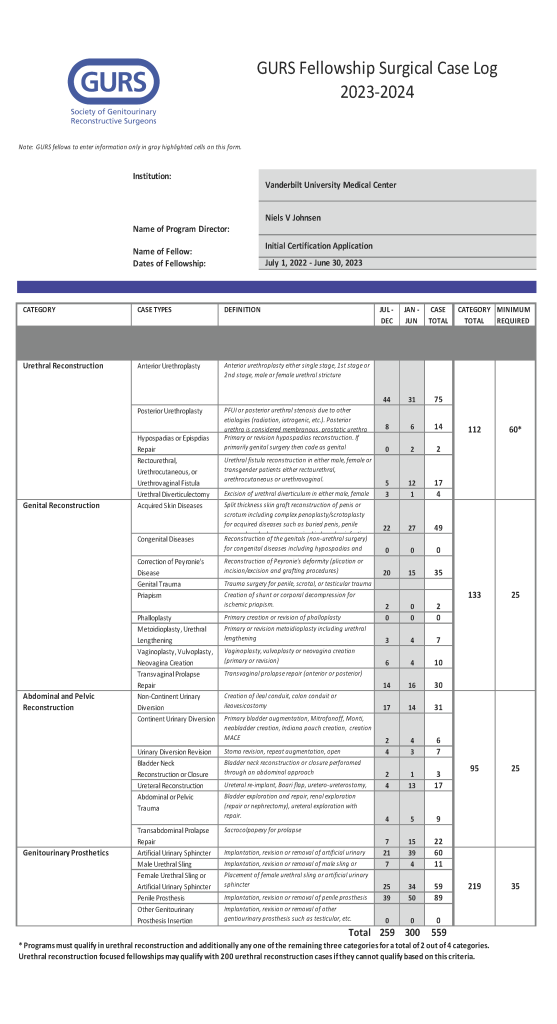
The clinical training encompasses all aspects of reconstruction for both men and women, as well as gender affirming surgery, through widespread surgical training in open, robotic, and transvaginal approaches. On the male reconstructive front, we offer extensive opportunities in anterior and posterior urethral reconstruction and rectourethral fistulae repair utilizing gracilis or other muscle flaps. Genital reconstruction is performed for lymphedema, hidradenitis, buried penis, genital malignancies, and following necrotizing soft tissue infections, where fellows will gain expertise in the utilization of various skin grafting and fasciocutaneous flap techniques. Fellows will also be exposed to a large clinical practice of post-prostatectomy incontinence and erectile dysfunction, as well as Peyronie’s disease.
The female pelvic health and voiding dysfunction component of the fellowship continues the great legacy of the Vanderbilt Female Pelvic Medicine fellowship initially founded by Roger Dmochowski in 2003 by providing unparalleled training in the management of female genitourinary reconstruction. Fellows gain extensive experience managing urinary incontinence and overactive bladder, voiding dysfunction, neurogenic bladder, genitourinary fistula and diverticula repair, pelvic organ prolapse, pelvic floor dysfunction, and neuromodulation. Procedures are performed both through transvaginal and transabdominal approaches, both robotic and open, preparing fellows to manage these conditions utilizing a variety of techniques.
Fellows will also gain extensive experience in the surgical management of bladder and upper tract reconstruction through robotic bladder neck reconstruction, bladder augmentation, open and robotic ureteral reconstruction, ileal ureter creation, as well as both continent and incontinent urinary diversions. Lastly, fellows have the opportunity to participate in our growing gender-affirming care program in conjunction with plastic surgery in vaginoplasty, metoidioplasty, and phalloplasty procedures.
Acute management and long-term survivorship care of genitourinary injury patients is a major component of the fellowship. With a graduated autonomy experience, fellows will direct the conservative and surgical management of GU trauma patients, coordinating closely with the general surgery and orthopaedics trauma teams.
The primary goal of the fellowship is to train future leaders in the world of reconstructive urology. Fellows are expected to complete scholarly work and contribute to the academic mission of the department by participating in Departmental conferences and didactics. Fellows are mentored through the development of research protocols, study design, statistical analysis and research dissemination and are expected to present their work at societal and national meetings.