Developing Tomorrow’s Leading Specialists
At Vanderbilt, we give you the clinical, surgical and administrative experience you’ll need to care for children with musculoskeletal diseases. As a pediatric level-one trauma center, we’re well positioned to provide you the opportunity to work alongside leaders in the field every day, treating a wide variety of acute pediatric orthopedic conditions.
And, as our fellow, you’ll have the support of top-of-field faculty and access to all of the resources that come with being a part of the Vanderbilt team. It’s our goal to ensure you’re equipped to move into patient care in an academic or private setting, and to join us in leading the way in pediatric orthopedic care regionally, nationally and internationally.
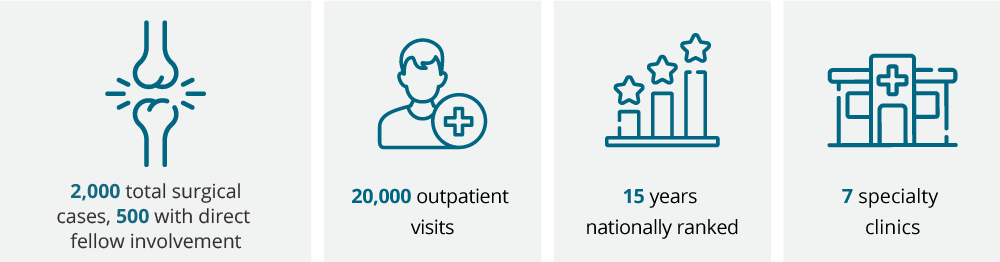
What We Do Here Every Year
Program Overview
Positions: 1 fellow
Duration and Dates: 1 year, Aug. 1 through July 31
Stipend: PGY6 level
Call: Every sixth weekend (cases only)
Location: Monroe Carell Jr. Children’s Hospital at Vanderbilt
Our staff works closely in conjunction with the departments of Neurology, Pediatrics, Rheumatology and Medical Genetics, and uses a combination of the most current and classic techniques to care for our patients. Some areas of special interest include the diagnosis and treatment of:
- Simple and complex fractures
- Musculoskeletal infections
- Scoliosis and other spinal deformities
- Pediatric and adolescent sports injuries
- Pediatric hip pathology, from infancy (DDH) through adolescence/early adulthood
- Clubfoot
- Congenital deformities of the hip, knee, and foot
- Orthopedic manifestations of pediatric neuromuscular disorders
- Leg length discrepancies
- Congenital hand and upper extremity conditions
- General treatment of bone tumors
As part of our POSNA- accredited (non-ACGME) fellowship program, you’ll work closely with faculty and staff at the Vanderbilt Department of Orthopaedic Surgery and Monroe Carell Jr. Children’s Hospital at Vanderbilt. Our children's hospital is an ACS Verified Level I Pediatric Trauma Center. We are one of 63 children's hospitals in the nation with Level I verification, and one of two pediatric trauma centers in Tennessee. You will also:
- Attend educational lectures
- Collaborate in bi-weekly pre-op and post-op case conferences
- Complete a research project worthy of publication or presentation at a national meeting
- Embrace basic science and clinical research opportunities
- Engage in monthly grand rounds and Morbidity and Mortality Conference
- Participate in our journal club
- Have the opportunity to attend to one funded national academic meeting conference (e.g. POSNA, IPOS)
Clinical Program
As a pediatric orthopaedic surgery fellow, you’ll be exposed to several thousand clinic patients during your fellowship year. As you learn to evaluate and manage musculoskeletal conditions in children, our faculty will provide you with critical feedback on your ability to assess surgical indications.
You will rotate with the attending surgeons in their clinic on a preceptor-based, one-to-one model, approximately one or two days each week. On Friday afternoons, you work in your own clinic, seeing a mix of new and post-op patients.
At the completion of your fellowship, you’ll be well versed in multiple subspecialty areas of pediatric orthopedics. You will gain a varied and thorough clinical experience and exposure to a full spectrum of pediatric musculoskeletal conditions and pathology.
Surgical Experience
As a fellow at Vanderbilt, you will participate in hundreds of cases over the course of your fellowship year. At the start of the program you will:
- Assist with preoperative planning on all cases you are involved in
- Participate in cases one-on-one with the attending surgeon, two to three days per week in the operating room
- Participate in postoperative management of operative cases, in conjunction with the orthopedic residents on the service
- Teach and provide guidance to residents on routine cases
As your fellowship year progresses, you are given a graduated amount of responsibility based on your skill level. We can tailor your experience to focus on the types of pediatric orthopedic cases you want exposure to before you go into practice.
Research Program
Fellows complete at least one clinical or basic science project of publishable quality under supervision a faculty member. You may be able to receive funding for your research from the Pediatric Orthopaedic Education fund, Brook's fund and other intra- and extramural sources.
Conferences and Workshops
Fellows complete a rigorous weekly and monthly schedule of conferences and workshops.
Weekly Conferences
Monday Pre-Operative Case Conferences
(6:30 a.m.)
Fellows and faculty review 100 percent of the operative cases for the week
Monday Didactic Lecture
(7 am, first, third, and fifth Mondays)
We focus on core competency topics. The attendings and fellow are assigned topics and the schedule is posted for the year. Power Point presentations are posted as enduring educational materials for resident and fellow education. Faculty provide discussion. The pediatric fellow and orthopedic residents are responsible for assigned readings prior to conference. Readings include but are not limited to:
- Green’s Skeletal Trauma in Children (Written by previous VUMC pediatric orthopaedic faculty Dr. Neil Green and currently edited by Dr. Gregory Mencio)
- Lovell and Winter's Pediatric Orthopaedics
- Rockwood and Wilkins’ Fractures in Children
- Tachdjian's Pediatric Orthopaedics
Friday Post-Operative Case Conferences
(6:30 a.m.)
Fellows and faculty review 100 percent of the operative cases for the week
Monthly Morbidity and Mortality Conference
The pediatric orthopaedic fellow and chief resident submit a list of all pediatric orthopaedic cases and any complications. They present selected cases with salient teaching points as supported by review of the pertinent literature on the topic.
Other Clubs and Activities
Anatomy Lab
This education lab is optional and available to pediatric orthopaedic fellows.
Journal Club
Our pediatric orthopaedic journal club meets every other month. Our fellow and chief resident on service coordinate with the attendings to select articles for discussion. Evidence-based medicine articles (preferably Level 1 or 2) are preferred. The pediatric orthopedic faculty provides expert opinion and practical clinical perspective during the discussion.
Monthly Orthopaedic Grand Rounds
Pediatric orthopaedic fellows attend when the topic is related to pediatrics.
Monthly Spine and Sports Medicine Conference
These conferences are available to pediatric orthopaedic fellows, but optional.
Sample Weekly Schedule
Monday
- 6:15 a.m. Pre-op Conference
- 7am Didactic Lecture every other week
- OR
Tuesday
- Attending Clinic
Wednesday
- OR
Thursday
- OR
Friday
- 6:15 .a.m Post-op conference
- 7 a.m. Grand Rounds/M+M
- AM—OR
- PM—Fellow Clinic
Application Process
We participate in the San Francisco match program. For more information about our fellowship program, contact Marla Johnson at (615) 936-2455 or email marla.johnson@vumc.org.
All applications must be submitted through the SF Match.
Please contact our Fellowship Administrator, Marla Johnson, for more information at Ortho-Fellowships@vumc.org.
In your subject line, please list which fellowship you are inquiring about.
Benefits
At Vanderbilt, we want you to enjoy a well-rounded fellowship experience. Benefits of our program include:
- Instructor status
- Two funded national conferences (POSNA, IPOS)
- Office with computer and workspace
- 24/7 exercise facility (free weight/aerobics) within our orthopedic surgery department
- Eligibility for health, vision, dental, disability, retirement and other benefits via open enrollment commensurate with a full time employed faculty member
- Four weeks of vacation (not to be taken in first or last 2 weeks of the academic year)
- Readily available orthopedic anatomy cadaver lab on medical campus
Our Current Fellow
 | Mitchell Scull, MD Hometown: Spartanburg, SC Undergrad: Clemson University Medical School: University of South Carolina - Greenville Residency: University of Tennessee – Chattanooga |
Our past fellows
2024-2025: Michael Burton, MD - currently practicing at Illinois Bone and Joint Institute, Chicago, IL
2023-2024: Kevin Serdahely, MD – Currently practicing at Cleveland Clinic, Cleveland
2022-2023: Courtney Baker, MD – Completed a second fellowship in Adult Reconstruction. Currently practicing at Vanderbilt University Medical Center/Monroe Carell in a dual role (Adult/Pediatric Hip), Nashville
2021-2022: Azlyn Goff, MD – Currently in private practice in Melbourne, Fla.
2020-2021: Nathaniel Lempert, MD – Currently practicing at Vanderbilt Children’s Hospital, Nashville
2019-2020: Jessica McQuerry, MD – Currently practicing at University of Florida Health, Gainesville, Fla.
2018-2019: Jeffrey Otte, MD – Currently practicing at Orthopaedic Institute of Ohio, Lima, Ohio.
2017-2018: Vince Prusick, MD – Currently practicing at Shriners Hospitals for Children, Lexington, Ky.
2016-2017: Cody Beaver, MD – Currently practicing at Cook Children's Hospital, Fort Worth, Texas
2015-2016: Holly Leshikar, MD – Currently practicing at UC Davis Children’s Hospital, Sacramento, Calif.
2014-2015: Phillip Mason, MD – Currently practicing at Novant Health Orthopaedics, Winston-Salem, N.C.
2013-2014: David Ebenezer, MD – Currently practicing at Vanderbilt Children’s Hospital, Nashville.
2012-2013: Kenneth Powell, MD – Currently practicing at Shriners Children's Hospital, Shreveport, La.
2011-2012: Michael Diab, MD – Currently practicing at Covenant Children’s Hospital, Lubbock, Texas.
Division Research
-
- C-Reactive Protein Predicts Risk of Venous Thromboembolism in Pediatric Musculoskeletal Infection. Amaro E, Marvi TK, Posey SL, Benvenuti MA, An TJ, Dale KM, Lovejoy SA, Martus JE, Johnson ME, Mencio GA, Moore-Lotridge SN, Thomsen IP, Schoenecker JG. J Pediatr Orthop. 2019 Jan;39(1):e62-e67. doi: 10.1097/BPO.0000000000001256. PMID: 30300275
- Effects of Antibiotic Timing on Culture Results and Clinical Outcomes in Pediatric Musculoskeletal Infection. Benvenuti MA, An TJ, Mignemi ME, Martus JE, Thomsen IP, Schoenecker JG. J Pediatr Orthop. 2019 Mar;39(3):158-162. doi: 10.1097/BPO.0000000000000884. PMID: 30730421
- Internal Rotation Stress Testing Improves Radiographic Outcomes of Type 3 Supracondylar Humerus Fractures. Bauer JM, Stutz CM, Schoenecker JG, Lovejoy SA, Mencio GA, Martus JE. J Pediatr Orthop. 2019 Jan;39(1):8-13. doi: 10.1097/BPO.0000000000000914. PMID: 27977497
- Pediatric Cervical Spine Clearance: A Consensus Statement and Algorithm from the Pediatric Cervical Spine Clearance Working Group. Herman MJ, Brown KO, Sponseller PD, Phillips JH, Petrucelli PM, Parikh DJ, Mody KS, Leonard JC, Moront M, Brockmeyer DL, Anderson RCE, Alder AC, Anderson JT, Bernstein RM, Booth TN, Braga BP, Cahill PJ, Joglar JM, Martus JE, Nesiama JO, Pahys JM, Rathjen KE, Riccio AI, Schulz JF, Stans AA, Shah MI, Warner WC Jr, Yaszay B. J Bone Joint Surg Am. 2019 Jan 2;101(1):e1. doi: 10.2106/JBJS.18.00217. PMID: 30601421
- Radiation Exposure During Operative Fixation of Pediatric Supracondylar Humerus Fractures: Is Lead Shielding Necessary? Martus JE, Hilmes MA, Grice JV, Stutz CM, Schoenecker JG, Lovejoy SA, Mencio GA. J Pediatr Orthop. 2018 May/Jun;38(5):249-253. doi: 10.1097/BPO.0000000000000810. PMID: 27280894
- The impact of curve severity on obstetric complications and regional anesthesia utilization in pregnant patients with adolescent idiopathic scoliosis: a preliminary analysis. Chan EW, Gannon SR, Shannon CN, Martus JE, Mencio GA, Bonfield CM. Neurosurg Focus. 2017 Oct;43(4):E4. doi: 10.3171/2017.7.FOCUS17321. PMID: 28965442
- X-ray vs. CT in identifying significant C-spine injuries in the pediatric population. Hale AT, Alvarado A, Bey AK, Pruthi S, Mencio GA, Bonfield CM, Martus JE, Naftel RP. Childs Nerv Syst. 2017 Nov;33(11):1977-1983. doi: 10.1007/s00381-017-3448-4. Epub 2017 Jun 27. PMID: 28656384
- Double-Edged Sword: Musculoskeletal Infection Provoked Acute Phase Response in Children. Benvenuti M, An T, Amaro E, Lovejoy S, Mencio G, Martus J, Mignemi M, Schoenecker JG. Orthop Clin North Am. 2017 Apr;48(2):181-197. Doi: 10.1016/j.ocl.2016.12.009. PMID: 28336041 Review.
- Similar Clinical Severity and Outcomes for Methicillin-Resistant and Methicillin-Susceptible Staphylococcus aureus Pediatric Musculoskeletal Infections. An TJ, Benvenuti MA, Mignemi ME, Martus J, Wood JB, Thomsen IP, Schoenecker JG. Open Forum Infect Dis. 2017 Feb 9;4(1):ofx013. doi: 10.1093/ofid/ofx013. eCollection 2017 Winter. PMID: 28480284
- Rigid Instrumentation for Neuromuscular Scoliosis Improves Deformity Correction Without Increasing Complications. Funk S, Lovejoy S, Mencio G, Martus J. Spine (Phila Pa 1976). 2016 Jan;41(1):46-52. doi: 10.1097/BRS.0000000000001170. PMID: 26352742
- Epidemiology, diagnosis, and treatment of pericapsular pyomyositis of the hip in children. Mignemi ME, Menge TJ, Cole HA, Mencio GA, Martus JE, Lovejoy S, Stutz CM, Schoenecker JG. J Pediatr Orthop. 2014 Apr-May;34(3):316-25. doi: 10.1097/BPO.0000000000000106. PMID: 24172679
- Twenty-Year Experience with Rigid Intramedullary Nailing of Femoral Shaft Fractures in Skeletally Immature Patients. Crosby SN Jr, Kim EJ, Koehler DM, Rohmiller MT, Mencio GA, Green NE, Lovejoy SA, Schoenecker JG, Martus JE. J Bone Joint Surg Am. 2014 Jul 2;96(13):1080-1089. doi: 10.2106/JBJS.M.01128. Epub 2014 Jul 2. PMID: 24990973
- Safety of topical vancomycin for pediatric spinal deformity: nontoxic serum levels with supratherapeutic drain levels. Armaghani SJ, Menge TJ, Lovejoy SA, Mencio GA, Martus JE. Spine (Phila Pa 1976). 2014 Sep 15;39(20):1683-7. doi:10.1097/BRS.0000000000000465. PMID: 24921849
- Complications and outcomes of diaphyseal forearm fracture intramedullary nailing: a comparison of pediatric and adolescent age groups. Martus JE, Preston RK, Schoenecker JG, Lovejoy SA, Green NE, Mencio GA. J Pediatr Orthop. 2013 Sep;33(6):598-607. doi: 10.1097/BPO.0b013e3182a11d3b. PMID: 23872805